EPISODE 58 | RELEASED May 29, 2020
Medicine for Dogs in Pain | Dr. Demian Dressler Deep Dive
Is your dog in pain, even though she’s not crying? Maybe! Is she anxious? Probably! Can you treat one without the other? Dr. Dressler brings us up to date on pain management for dogs.
SHOW NOTES
This is a must-listen Deep Dive episode, where Dr. Dressler covers the ins and outs of pharmaceutical and herbal approaches to pain management, as well as hands-on techniques.
Dr. Dressler is co-author of our podcast sponsor, the book The Dog Cancer Survival Guide: Full Spectrum Treatments to Optimize Your Dog’s Life Quality and Longevity.
The Glasgow Composite Pain Scale can be found here: https://www.newmetrica.com/wp-content/uploads/2016/09/Reid-et-al-2007.pdf
Pharmaceuticals mentioned in today’s episode:
- Tramadol
- Tylenol with codeine
- Hydrocodone
- Oral hydromorphine
- Fentanyl
- Gabapentin
- Metacam
- Carprofen
- Deramaxx (deracoxib)
- Previcox
Non-Pharmaceuticals mentioned in today’s episode:
- Apocaps CX
- Traumeel
- EverPup
- Nutrocept
- glycosaminoglycans
Other pain management strategies:
- Hydrotherapy, warm and cool
- Massage
- Acupressure
- Acupuncture
You can reach out to Dr. Demian Dressler directly on his veterinary hospital’s website: https://VetinKihei.com.
>> Dr. Demian Dressler: One of the most common ones these days is Tramadol. Also Tylenol with codeine, hydrocodone, oral hydromorphine, fentanyl patches — those are the biggies that are used these days. So the question is, well, why are these medications being used for pain when they’re not reliable pain controls?
>> Announcer: Welcome to Dog Cancer Answers where we help you help your dog with cancer. Here’s your host, James Jacobson.
>> James Jacobson: Thank you for hitting that play button. Today’s episode will make it well worth your while, because we are delving into a very nuanced topic that is of utmost importance for anyone dealing with dog cancer: and that is pain control.
Things have changed over the last couple of years when it comes to helping our dogs with pain, and as always, Dr. Dressler has thoughts based on both the literature and on treating dogs in his own practice. Let’s dive right in…
Dr Demian Dressler is co-author of the bestselling book, The Dog Cancer Survival Guide. He is a graduate of the Cornell School of Veterinary Medicine, and he’s been in private practice since 1997. Dr. Dressler, welcome to the show.
>> Dr. Demian Dressler: Thank you.
>> James Jacobson: Today we’re going to talk about pain and how to manage your dog’s pain because pain, I guess, is a big part of many types of cancer.
>> Dr. Demian Dressler: It is. It’s a really negative life quality thing and one of the big parts in cancer care in general, and I go over this, when people call me for answers, considering their dog’s care, how do we maximize both life quality and also longevity?
>> James Jacobson: Well, why is it confusing? I mean, it’s obvious you need to do something for your dog’s pain, but it can be a confusing topic.
>> Dr. Demian Dressler: Well, sometimes people will conflate pain with other negative life experiences, and maybe they’re related, but they’re not exactly the same thing. Because when you’re treating pain, you’re getting rid of a very specific physiological phenomenon with pain control efforts. And there can be drugs and therapeutics and homeopathics and all these different ways to address pain, but we need to be careful.
Is it pain or is it low energy? Is it nausea? Is it flu-like symptoms? Those are all kind of related to pain, but guess what? If you treat those other things with pain control efforts, you’re not going to do the best thing for the dog. It’s not going to work.
>> James Jacobson: So how do you know if your dog is in pain?
>> Dr. Demian Dressler: Well, there’s the scale that’s developed to assess this, and it’s called the Glasgow Composite Measures Scale.
And the reason why that was developed was because we can’t look at yipping and crying and vocalizing as a very reliable hallmark of pain because it turns out that other things can cause yipping and crying and vocalizing, such as anxiety. And it also turns out that dogs that are in pain may not yip, cry or vocalize.
So we have to look at other things in addition to that.
>> James Jacobson: So on that last point, I understand that if a dog is yipping, it could be because there’s separation anxiety or a myriad of other reasons. But you’re saying sometimes when they’re in pain, they don’t vocalize?
>> Dr. Demian Dressler: Absolutely true. A lot of it has to do with degree and how chronic it is or how acute it is. So if something is acute, it’s happening very quickly. So if you get stung by a bee there’s a good chance, you’ll say, ow.
>> James Jacobson: Right.
>> Dr. Demian Dressler: However, if you’ve got that same degree of pain over a month, you’re not going to probably walk around going ow, ow, ow, ow, ow, ow,
>> James Jacobson: It’s the frog and the boiling water thing.
>> Dr. Demian Dressler: Yeah. And the body will try to suppress the pain and also due to the fact that it’s happening all the time, you’re not going to vocalize, neither do dogs. So dogs that are in chronic pain actually very rarely vocalize, unless it jumps up in magnitude, it goes above the existing threshold. Then they’re going to yip and vocalize. So that’s why we don’t see vocalization necessarily in dogs that’re in pain, a lot of times there’s other signs.
>> James Jacobson: So talk about this Glasgow thing. What is this Glasgow thing? It sounds like it’s very, very proper,
>> Dr. Demian Dressler: Well, that’s cause it was developed in Glasgow, it sounds pretty good. And so that’s where the composite pain score was developed, both on the human side and on the animal side.
>> James Jacobson: Is this like when you go to the hospital and they say on a scale of one to 10 and you’re obviously asking the person. How bad is it?
>> Dr. Demian Dressler: Right? So that’s a simplified sort of
>> James Jacobson: So you can’t do that for a dog.
>> Dr. Demian Dressler: Right. So what they’ve done is they look at all of the possible signs of pain and then you get a score, and that way you’re able to assess, okay, well do we have to do pain control or do we have to not do pain control based on these more reliable signs of pain? And when you look at multiple things in conjunction, that gives you a clearer idea as opposed to just one, like vocalization.
So for example, whimpering, crying, groaning, screaming. Okay. Got it. Sometimes that can be associated with pain, but it’s sometimes not.
Now, sometimes a dog will look at the painful area, will rub at it, will lick it, chew it. Okay. That can be another possible sign of pain, but guess what? Not every time.
How bout limping? Well, that’s usually pain. Moving around slowly. Reluctance to move. If you push the painful area and they respond, they look back or they snap or they move away, that’s another sign. Interestingly, being depressed, nervous, or anxious, that can also be a sign of pain, but not always.
And then kind of test and having a hunched posture, like sometimes they’ll guard the painful area, but if, for example, if you just look at a dog who has a hunched posture, that’s not a reliable sign of pain.
So you add all of these things up and it’s either a five or a six, beyond that — out of 24 — you got to do pain control and those are the guidelines, and if the animal is bedridden, all you need is a five and if the animal is not better then you do a six because lying around is one of the criteria that you look at.
>> James Jacobson: You recently wrote a blog post about this, and you can get a link to that in the show notes for this episode at DogCancerAnswers.com/pain. And you pointed out that there are many commonly prescribed medications that aren’t actually quite effective.
>> Dr. Demian Dressler: That’s right.
>> James Jacobson: What are they and why?
>> Dr. Demian Dressler: Well, there’s a lot of them, but the one of the most common ones these days is Tramadol. Also Tylenol with codeine, hydrocodone, oral hydromorphine, fentanyl patches — those are the biggies that are used these days. So the question is, well, why are these medications being used for pain when they’re not reliable pain controls?
>> James Jacobson: Yeah. Why?
>> Dr. Demian Dressler: Well, the — a couple of different reasons. One is because the research that is now available that shows that it’s true. That’s one reason, and it wasn’t available when the drug first came out.
>> James Jacobson: Wait a second. So the drugs came out because they showed that they were effective, and then there’s new research now that shows that they’re not effective, but the drugs are still being used.
>> Dr. Demian Dressler: Right.
>> James Jacobson: Okay. Great!
>> Dr. Demian Dressler: Yeah. Which I think informs the fact that pain assessment is, number one difficult, and the measurement of it gets more and more sophisticated over time.
So it’s not an easy thing to measure.
And the second thing is the population numbers, like test numbers. So when you’re doing a pharmaceutical, I think it’s 40 dogs or something as the minimum, somewhere around there. And then that’s pretty different from multiple studies involving many different locations.
And so the numbers go up. And so if you have a larger population, you see things that are more true because you’ve got more examples of it.
>> James Jacobson: Okay. So there’s new research that shows maybe not so effective. What else? What are the reasons why these medicines?
>> Dr. Demian Dressler: Oh, I’d say institutional inertia. So doctors are not very good — I’m included in this, by the way — at sometimes, looking at information that tells them that what they’re doing is wrong. So there’s a resistance there. And a matter of fact, I was just discussing this with a consulting client the other day. It was like, “Oh, yeah, I’ve got it. I’ve got my pain control. You know, we’ve got our Tramadol and our Gabapentin and stuff.”
And I’m like, “Well, umm, sorry, that doesn’t really do very much for pain.” And she was a little bit taken aback because she had heard from her veterinarian that this is a good pain control drug. And it, you know, it does help somewhat some of the time, but not as reliable as we need.
And we look at pain control, and a big part of pain control in dogs as it turns out, is anxiety control.
>> James Jacobson: Hmm.
>> Dr. Demian Dressler: Dogs and people, by the way, experience anxiety connected with pain. It’s a related but distinct phenomenon because when you’re anxious, you’re not necessarily painful, but those two things can be linked. If you have chronic anxiety, you can create painful conditions, and if you have chronic or acute pain, you can have anxiety.
So they’re connected.
Now what those drugs do pretty darn well is alleviate anxiety. And if you look at like the narcotics, for example, and if you look at things like Tramadol, and in some cases Gabapentin and hydrocodone and all that, they have sedating effects and/or anti-anxiety effects.
>> James Jacobson: So that’s what people are seeing is their dog isn’t anxious, but not — their pain may still be there, but they’re just like too groggy to — some
>> Dr. Demian Dressler: Well, that’s a piece of it that could happen. And then also they could be a dog who is really not feeling all that much pain, but has muscle tension and anxiety-related signs and it actually, the anxiety is the real issue. And dogs that have anxiety also, that’s pretty tough to measure. Just like it is in people.
It’s pretty tough to measure unless somebody says, “I have anxiety.”
>> James Jacobson: Okay. I think you’ve opened up something that I want to explore, which is really what is pain? Cause clearly you’re making the distinction between anxiety, some of these medications deal with and treat, but then what actually is pain?
>> Dr. Demian Dressler: That is a very good question.
A very deep one because it gets pretty philosophical pretty quickly. So from a scientific standpoint, pain is defined as the stimulation of modified nerve ending cells that are called nociceptors, that respond to noxious stimuli such as trauma, such as chemical, such as heat, and these are destructive phenomenon on the body.
Okay? So these modified little cells are capable of sensing that. And they’re connected with nerves and those nerves relay signals that go up into the spinal cord and then up into the brain and are connected with certain parts of the brain and fire in certain patterns that the brain then perceives as the experience of pain.
>> James Jacobson: So that’s where the pain is actually being registered is in the brain.
>> Dr. Demian Dressler: Right.
>> James Jacobson: But it’s started at wherever, the point is where these what are these,
>> Dr. Demian Dressler: They’re called nociceptors.
>> James Jacobson: Nociceptors are triggered. Okay. So. It’s a brain thing. So don’t some of these drugs just basically interfere with the brain’s ability to receive this noticeptors or, or
>> Dr. Demian Dressler: Nociceptors? Nociceptors. Yeah. Right. So that’s what a good pain control medication is supposed to do. It’s supposed to somehow block that somewhere, and it doesn’t have to happen in the brain. Like when you get a shot of Novocaine at the dentist, it can happen locally where the nociceptors are. That’s what lidocaine does. and bupivacaine and those drugs and you don’t feel pain there. Matter of fact, you don’t feel hardly anything at all. But that’s how you can get oral surgery done without being anesthetized because your brain is perfectly awake. But those signals are getting squashed right where they start. So then you have also the central processing of it, which is occurring in the head, and that’s where the experience of pain is occurring.
And when you take a pill it’s operating mainly up in the central nervous system, which is the brain and spinal cord.
>> James Jacobson: Okay. Some of these are basically probably just treating anxiety as not so much the pain.
>> Dr. Demian Dressler: Right.
>> James Jacobson: Anxiety is obviously also in the brain. So you’re saying that some of these commonly used pain medications, it’s now showing are treating the anxiety but not the pain. So the dog is still feeling the pain. They’re just not expressing it.
>> Dr. Demian Dressler: We don’t really quite know cause it’s hard to differentiate those two things. So what’s the salient feature? The salient feature is we want to avoid a circumstance where we’re not giving good pain control.
And instead in that exact predicament that you just described where we’re sedating an animal, and then having it actually still be in pain, but we could avoid the sedative and instead control the pain without the sedative. So that’s a nice way of doing it. If you give less drugs, you’re generally better. Often, however, we’ll see — what’ll happen is the pain is not very well controlled, then you start ratcheting up the sedative effort more and more and more. And it’ll appear as if the pain is controlled, the heart rate will go down, the animals start to sleep and stuff like that. But we’re giving more and more drugs that kind of has this peripheral effect of putting the dog to sleep basically.
And we could be handling it much more gracefully and much more healthful fashion by using less pharmaceuticals that are more specifically pinpointed towards what’s going on.
>> James Jacobson: And we’ll get to that in a minute, cause I know you have some recommendations, but what about opioids? Because opioids is obviously all over the headlines, it’s way over-used and -prescribed in human medicine. Is there a similar thing in veterinary medicine?
>> Dr. Demian Dressler: Yeah, well, the drugs that I just mentioned mainly are narcotics, which are opioids.
>> James Jacobson: All of them.
>> Dr. Demian Dressler: Yeah, Tramadol is in that family. Codeine is in the family. Hydrocodone is in the family. Hydromorphone, fentanyl. These are all opioids.
>> James Jacobson: Okay. So this is literally the same thing that we’re seeing mirrored in, but these are not addictive, or codeine’s addictive?
>> Dr. Demian Dressler: No, they’re addictive.
>> James Jacobson: They all are. Okay. Let’s talk more about that when we come back from our break.
Today’s episode of Dog Cancer Answers is brought to you by the best-selling animal health book, The Dog Cancer Survival Guide: Full Spectrum Treatments to Optimize Your Dog’s Life Quality and Longevity by Dr. Demian Dressler, our guest on today’s show, and Dr. Susan Ettinger (an oncologist in New York). And in a minute I will tell you how to get their book at a discount.
As you’re hearing in today’s show, Dr. Dressler is truly a “Full Spectrum” veterinarian. That means he doesn’t waste time with dogma. If something is helpful and it’s from big pharma, it’s in the book. On the other hand, if something is helpful and it’s from a different medical tradition, or even is just a lifestyle change, it is in the book. What you get is no polarization, just information about all the things that have been shown to work in dogs with cancer. And I can tell you from firsthand personal experience, that this is invaluable.
The Dog Cancer Survival Guide is available wherever fine books are sold — both online and in physical bookstores. And you can support this podcast by using a coupon code and getting The Dog Cancer Survival Guide right away direct from the publisher. It is available either in paperback (and there is free shipping to the US address, any US address), or as an e-book edition that is under ten dollars.
The website to get either the paperback or the ebook is www.DogCancerBook.com.
And you will save 10%… if you use the promo code “podcast” when you check out, you will save 10%. The website again: DogCancerBook.com. Use the promo code “podcast” for 10% off. That is www.DogCancerBook.com.
And, we’re back, what about opioids?
>> Dr. Demian Dressler: Well, the drugs that I just mentioned mainly are narcotics, these are all opioids.
>> James Jacobson: But these are not addictive, or are they?
>> Dr. Demian Dressler: How do you define addiction when you’re, when you’re dealing with a dog, you know, we don’t really recognize withdrawal very well, like as an entity in veterinary medicine.
I bet you if we’d started looking at that, we would see evidence of that. Like, because that’s kind of the hallmark of addiction is withdrawal. That’s how you really can see it. So that would be an interesting thing to look at. But we don’t have the information yet.
>> James Jacobson: Dogs are jonesing for codeine or whatever. Tramadol,
>> Dr. Demian Dressler: Yeah, maybe being lethargic, sick, unhappy, nonresponsive, and just laying around and isolating and you know, doing all that. That’d be pretty interesting.
>> James Jacobson: Okay, so the question is. What do you recommend?
>> Dr. Demian Dressler: Right. So one of the big pieces here is we can’t start using things that are unreliable for pain control and also cause sedative, or anti-anxiety effects as sole agents.
That’s the thing. If you reach for that as those are single drugs, that’s a mistake. So instead what we want to do is the anti-inflammatory drugs. Rely on those and then use these other drugs as ancillary or add-on pain control efforts if we’re going to be looking at pills or shots and we’re doing conventional care.
So what do I mean by the anti-inflammatories? Well, those are going to be things like Metacam. Those are going to be things like Carprofen. Those are going to be things like Deramaxx which is deracoxib. Previcox. There’s a whole family of these things. They’re pain relieving anti-inflammatory drugs. It turns out that those actually do a pretty darn good job on dogs that are in pain in terms of the pain effect, and then clarifying what we’re doing with the other drugs, such as the Gabapentin, such as the Tramadol and such as these other drugs, and not using those all by themselves.
So if we create a combination where — if we’re doing conventional care, that is — and we’re using pharmaceuticals, we’re going to be using a nonsteroidal anti-inflammatory drug as the main pain relief, and then combining that if necessary with something that helps with anxiety and/or wind up.
And what gets really crazy? Wind up is something that I see in dogs and it is described in dogs, and you’re probably going to ask What is wind up? So wind up is a piece of the pain phenomenon that is connected with chronic exposure, like the painful thing is happening over a long period of time. So there’s two basic directions that our body will go when it’s experiencing that.
One is the body will start to suppress the pain through its own natural mechanism, so the sensation of pain goes down, things become tolerable, even though the pain thing is still there, you just live with it and then it goes away.
Oh, cool.
So you know, you could do like meditation and stuff like that, and the body does that naturally on its own.
Now it can go the opposite direction, and this is usually more with people who have dogs who have anxiety issues. They’re usually more sensitive, they’re less able to cope with challenges and all that, and they have anxiety issues.
They can go in the other direction, which is wind up. Which is they get sensitized to it and it gets worse and worse and worse and worse and worse. And then over time they’re just freaking out. And that’s got to do with exactly as it sounds, this winding up phenomenon, which is this basically this anxiety and stress response that goes in little circles in their minds, like a clock going around and around,
>> James Jacobson: Right.
>> Dr. Demian Dressler: And so the pain, the experience of pain in these individuals is worse then it would be
>> James Jacobson: And it gets progressively worse as time goes on.
>> Dr. Demian Dressler: It can. It doesn’t have to, but it can. And so you use drugs like Gabapentin for that. And I think that’s also how some of these other drugs are working too. That’s the anxiety connection.
And you talk to people and they’re experiencing legitimate pain that’s worse, but it’s because of the windup.
>> James Jacobson: Okay. What else do you suggest for pain?
>> Dr. Demian Dressler: Okay, so when you look at pain, it’s a broad subject, and so we don’t have to always do conventional care. Right? Especially chronic pain. So we’ve got our drugs, we’ve got our pharmaceuticals.
We use those as needed. So we can also do, for example, natural anti-inflammatories. That was one of the reasons why I put the Cox-2 inhibitors in Apocaps. Those are natural anti-inflammatories, so that’s a nice thing to do and that does have effect. It’s not as quick as the drugs, takes a couple of weeks.
But yeah, those will kick in. That’s why a lot of people, you know, that I talked to on the phone will call and they’ll be like, my dog was limping all over the place and now he’s jumping around like a puppy. Well, guess what? You’re doing a natural anti-inflammatory. So that’s a nice way to do it. And we can also do things like massage that can help a lot.
Also, heat and cold can help a lot. And these are going to be with warm compresses or cool compresses. Acupressure at home. For particularly chronic pain that can help a lot. That’s where you massage with your finger areas that are acupuncture stimulating points. Acupuncture is another way to do it. So kind of that’s the brief synopsis of other ways to address pain.
>> James Jacobson: Okay. And a lot of vets are doing acupuncture these days.
>> Dr. Demian Dressler: Oh yeah. Acupuncture is now becoming a much more accepted modality. Although I did talk to somebody the other day whose dog it was having disc problems and you know, I do acupuncture all the time, a certain type of it, and he’s like, I don’t believe in that.
I was like, well, okay, then.
>> James Jacobson: Okay, so it is, it’s seeing is believing, right?
>> Dr. Demian Dressler: Yup.
>> James Jacobson: Okay. So acupuncture, the cold compresses and cold and warm — so do you go back and forth?
>> Dr. Demian Dressler: So how do you know what to do? So the rule of thumb in general is if something is cool, cold, you warm it. And if something is warm, in general, you cool it.
>> James Jacobson: Okay. So how do you know if
>> Dr. Demian Dressler: You put your finger on it and then you touch the other area next to it.
>> James Jacobson: Interesting.
>> Dr. Demian Dressler: Yeah. And you can tell the temperature change.
>> James Jacobson: So what’s an example of something, maybe related to cancer where it would be cooler that you would use a warm compress on.
>> Dr. Demian Dressler: So those are going to be usually areas that are not in the area of the tumor, but where the animal is having orthopedic problems, and those are chronic. And so they’ll be stiff and the range of motion will go down.
So you’ll have, as an example, a dog who’s got an osteosarcoma bone tumor, say of the front leg in the radius ,above the elbow. So that area will feel kind of warm and hot, again, it’s not moving well, right? Well, it’s limping for a while now, and so now its back is starting to hurt because it’s bearing weight strangely. And so you feel on the back, it’s stiff and cool. That’s along the back. The reason why is because the back is all now messed up. So now you’ve got two reasons for pain.
So that would be an area for warmth and massage and traction and stuff like that.
>> James Jacobson: So how do you make a compress.
>> Dr. Demian Dressler: Oh, well you take a cloth
>> James Jacobson: Like a washcloth or
>> Dr. Demian Dressler: Yeah, it’s pretty basic, or a tee shirt or something like that. Absorbent fabric. And you can do a couple of different things there. You can just do warm water, which is kind of nice, like a bath sort of temperature.
You can also buy these little beads, these little pillow beads that you can put in your microwave. You can do a hot water bottles and we can do that. So those are all warm compresses. And so whatever you do for your dog, you want to touch yourself, you know, your skin on your forearm, so you get an idea of what you’re doing.
So something to keep in mind, too. You don’t want to kind of get them too — some of these old big dogs who are lying around a lot, get pretty hot on their pillow beds. So stick your hand underneath their bodies and feel the temperature there between the dog’s torso and the pillow bed. Because sometimes they’ll be getting really hot and it will be surprisingly hot.
And you gotta be careful if you’re heating an area, like they’re already really hot and then you’re applying this other heat to a different area. And it’s like, you know, it can be a little bit much. So be sensitive to that.
>> James Jacobson: And a cool compress, or do you use ice, or?
>> Dr. Demian Dressler: You can use crushed and then you got to put it in a Ziploc or something like that, and then you wrap it in a soft cloth that’s damp.
That’s one way to do it. You can always use frozen peas and carrots. You can do that. Again, soft damp fabric
>> James Jacobson: Protecting the icy thing, whether it’s vegetables or ice,
>> Dr. Demian Dressler: Right, and then there’s blue ice as a nice thing to do. You keep those in your freezer and they’re soft and malleable, and then there’s a lot of really cool, nice, if you want to really get into it, you do these circulating water cuffs, I can’t quite remember what they’re called, but it’s a hydrotherapy and they circulate water through these cuffs that you can attach to body parts and they’ve got this little pump that cools them off and the water is continually recycled and cooled down as it circulates through this thing that contacts the skin.
>> James Jacobson: And acupressure, how do you learn to do that?
>> Dr. Demian Dressler: Well, you got to know the points, right?
>> James Jacobson: Is this YouTube just go to YouTube? There’s gotta be a lesson out there.
>> Dr. Demian Dressler: I know there’s a book out there and uh, I think it’s called Dog Acupressure. I can’t remember the author. One of the easiest things to do if you know how to give a person a massage is you give your dog a massage.
And cause I have found over the time that I’ve been doing this, that the stimulation of myofascial trigger points versus acupressure points and acupuncture points, which technically are different, turns out to yield a lot of the same benefit. So what I’ll usually do is I’ll usually do acupuncture in myofascial trigger points.
So a trigger point is simply an area, and you can find one very easily. If you look on your hand and you look at the skin fold between your thumb and your index finger, there’s a skin fold. If you open your hand it stretches. If you pinch that between your thumb and your forefinger and you reach up towards the bone, you’ll feel a little blip, and that little blip almost always will have a pain in it. That’s a trigger point.
Okay. It turns out that dogs have the exact same phenomenon in their bodies, and you can start to feel them with your finger. They’ll feel like little knots of fibrous connective tissue, little balls, a firm something — that are about the size of an eraser or pea or something — and the areas that you look at will be the exact same areas many times that a person would feel stiff and sore, that’s going to be along the back and on the legs. It’s exactly where you would intuitively reach for when you’re giving somebody a massage.
Don’t poke your dog with your like, jab them with your fingers.
You use soft pressure and you can feel them and your finger will naturally settle in. You’ll feel the spaces by the way, and your fingers will settle in there. You can start to drag circular motions or softly, you do a massage and it turns out that these trigger point pressure seems to create a lot of the same benefits as acupressure or acupuncture, and you can do that just by being sensitive at home.
>> James Jacobson: Okay. Anything else? Injections?
>> Dr. Demian Dressler: That’s on the pharmaceutical side.
>> James Jacobson: Obviously it kind of demonstrates why you’re the full spectrum vet. I mean, this is like, you know, we’re going from opioids to acupressure to, what about injections?
>> Dr. Demian Dressler: Yeah, so an injection is something that usually a veterinarian will be handling.
It’s going to be probably outside the domain of control of most guardians. The injections that are given at home are typically those where the animal is really having a hard time going in and out of the practice and they’re non-controlled substances like anti-inflammatories and we teach guardians how to do that at home.
You can do it. You can do it. It’s not so bad if it’s under the skin. You can give injections under the skin and the muscle or in a vein. Under the skin is not so bad for most dogs. It’s not that painful. Many times it’s not at all. So we can give it pharmaceuticals, we can give drugs like that, and these are going to be, again, the anti-inflammatories that I’ve mentioned before.
It can be given like that. Also, we have an injectable called Traumeel, which has arnica and some other things in it and that’s from Eastern Europe. I use that a lot actually. So it’s kind of a natural anti-inflammatory that’s injectable, rapid-acting, works pretty good. Moderate in terms of its effect.
And then sometimes we’ll give cartilage drugs, glycosaminoglycans that have some pain-relieving effects for the orthopedic problems.
So that’s kind of like really souped up glucosamine chondroitin or something like that. Kind of like what we put in supplements EverPup and Nutrocept, so these are going to be your joint, your orthopedic types of compounds, and if you give them by injection, you’re giving a whole bunch. Like a really a lot, and that has more of an effect, and that’s where we’re using natural compounds more like quote unquote drugs, because the amount is so high and the purity is so high. You see the same thing in people when you get like B vitamin injections, it’s kind of like the difference between getting a B shot at the doctor versus taking a B vitamin at home. There’s a difference in the effect.
It’s much more amplified. So we’ll do that sometimes for pain control and dogs using glycosaminoglycans.
>> James Jacobson: Wow. There’s a lot to do for uh, pain management for dogs. A lot of solutions all over the gamut, and your blog post is great. If you want to link to that, you can find it in the show notes for this episode at DogCancerAnswers.com/pain. Dr. Dressler, thank you.
>> Dr. Demian Dressler: Thank you.
>> James Jacobson: So, listener, that is our massive episode on the newest thinking in pain management. I know I learned a lot. One takeaway that I have is this: science is always evolving. The pain management tools that we once thought were fantastic turn out, once they are used clinically for a few years, to not be as helpful as we thought they might be.
So, always check in with yourself and with your dog, right? As Dr. D mentioned, doing non-medical things might be, I think he said “more graceful” for your dog. For example, I know for sure that I used to think that my dog Maui loved Tramadol, because it seemed to take her pain away. But listening to Dr. D during our conversation, I wondered to myself whether in fact she was just groggy, not really pain-free.
I’ll never know, and I’m not going to beat myself up about it, because now I know better, I’ll do better. And my dog Roo, who has a lot of anxiety, might actually really LIKE Tramadol for its sedative effects, so I’ll remember that if we ever need to use pain meds for her. (Knock on wood)
The point is, our dogs are individuals, and what works for one dog might not for another. So check in with the Glasgow scale on your own dog (links are in the show notes) and keep track. Don’t assume that just because you’re giving a medication it’s working. If your dog seems like they aren’t getting any better, tell your veterinarian so they can help make adjustments.
We’re always learning, right? Well, definitely read Dr. Dressler’s article on pain management, which will be updated as time goes by if things change.
Links to that are in the shownotes, which are in the podcast app you’re listening to now, or at the following link: DogCancerAnswers.com/pain.
If you’re enjoying Dog Cancer Answers, the best way that you can help support this free podcast for dog lovers facing dog cancer is to subscribe in the app of your choice and tell a friend or even your own veterinarian about the show. The more ratings, and reviews, and listens, and subscriptions that we get, the higher we’re ranked, and the more likely other people are to find us just when they really need us.
And hey, if your personal veterinarian is like our other veterinary guests, maybe they should be on the show. Next time you see them, maybe plant the idea that they could be destined for greatness –or at least for a guest slot on our program. All they have to do is contact our producers via our website at DogCancerAnswers.com.
<<TOUCH TONE SFX>>
It’s those touch tones which remind me to remind you that our veterinarians are “on-call” at our Listener Line. If you have a question for a dog cancer vet, please call our listener line and record your question. We will pose it to one of our veterinary experts (and as a little experiment for a limited time only — we’ll actually email you the vet’s answer to your question as soon as we have it). After that, your question and the answer will appear on a future episode of Dog Cancer Answers. The telephone number for the listener line: 808-868-3200 or you can visit our website at DogCancerAnswers.com.
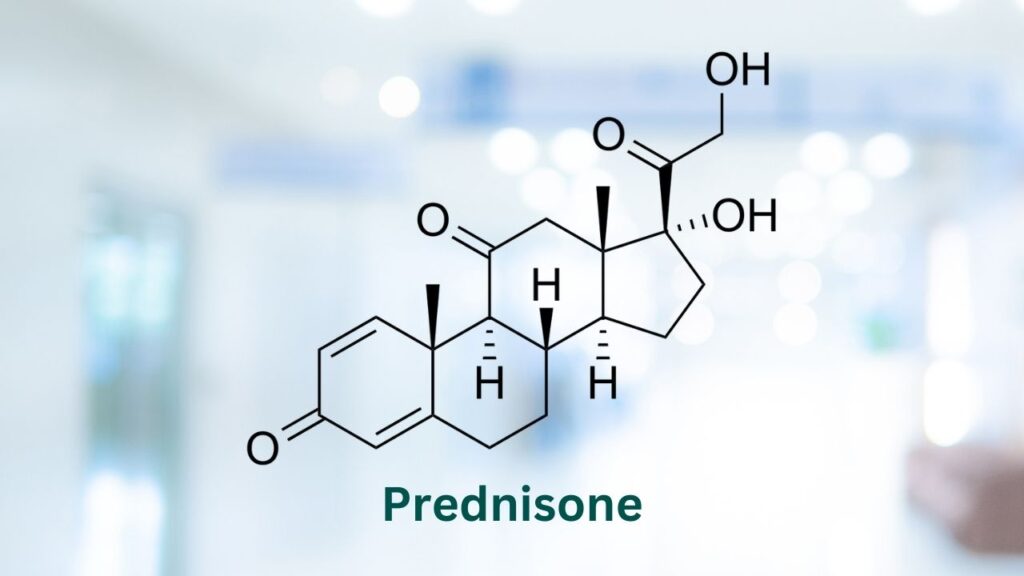
And in a moment I will tell you about our next deep dive episode about prednisone, but first…
We would like to take a moment to thank our sponsor: The Dog Cancer Survival Guide book by Demian Dressler and Sue Ettinger. The book is available wherever fine books are sold both online and in physical bookstores. And remember, if you would like to help support this podcast, get the book today — direct from the publisher, Maui Media. The website again: DogCancerBook.com. Use the promo code “podcast” for 10% off when you check out. That is www.DogCancerBook.com.
On our next deep dive episode of Dog Cancer Answers, we’re talking to Dr. Tammy Powell about everything Prednisone: it’s uses, it’s benefits, and its side effects, both short term and long term. Prednisone is a drug that is used for LOTS of things, not just cancer, so it’s another can’t-miss episode.
And the best way to make sure that you get it as soon as the episode is released is to subscribe to Dog Cancer Answers in Apple Podcasts or your favorite podcast app. We are also on Spotify and YouTube.
I’d like to thank Dr. Demian Dressler for being our guest today. If you would like to reach out to him, here is his website: vetinkihei.com
Until next time, I am James Jacobson. From all of us here at Dog Cancer Answers, & Dog Podcast Network–I wish you and your dog a warm Aloha.
>> Announcer: Thank you for listening to Dog Cancer Answers. If you’d like to connect, please visit our website at DogCancerAnswers.com or call our Listener Line at 808-868-3200.
And here’s a friendly reminder that you probably already know: this podcast is provided for informational and educational purposes only. It’s not meant to take the place of the advice you receive from your dog’s veterinarian. Only veterinarians who examine your dog can give you veterinary advice or diagnose your dog’s medical condition. Your reliance on the information you hear on this podcast is solely at your own risk. If your dog has a specific health problem, contact your veterinarian.
Also, please keep in mind that veterinary information can change rapidly. Therefore, some information may be out of date.
Dog Cancer Answers is a presentation of Maui Media in association with Dog Podcast Network.
Hosted By
SUBSCRIBE ON YOUR FAVORITE PLATFORM
Topics
Editor's Picks
CATEGORY