EPISODE 241 | RELEASED March 18, 2024
Palladia for Dogs | Dr. Megan Duffy
Veterinary oncologists are using the drug Palladia for dogs with many types of cancer now. Dr. Megan Duffy explains why.
SHOW NOTES
Is Palladia safe? Does it have a lot of side effects? Does giving my dog a cancer drug at home multiple times a week make my dog “toxic”? Can my dog with other health problems take this drug safely?
Palladia was approved for dogs with high-grade mast cell tumors in dogs over a decade ago. But since then, veterinary oncologists have started using it in many solid tumor types. They’ve also tweaked the doses to lessen the risk of side effects.
Veterinary oncologist Dr. Megan Duffy joins us for an in-depth look at this “kind of weird, exciting drug.” She explains a little about how it works, when it is used, and answers ALL the questions that came up in our Facebook Dog Cancer Support Group about this drug.
If your veterinarian wants to start your dog on Palladia, and you’re wondering why … this is a must-watch video for you because Dr. Duffy has advice about how to know if Palladia might help YOUR dog’s case.
Join our Facebook support group at https://dogcancer.com/support
Call +1 808-868-3200 to leave a question on our Listener Line for a future show!
>> James Jacobson: [00:00:00] Your vet is recommending Palladia for your dog’s cancer. Will it help? Are there side effects? Let’s talk to veterinary oncologist Megan Duffy and find out all about Palladia for dogs.
>> Announcer: Welcome to Dog Cancer Answers, where we help you help your dog with cancer.
>> James Jacobson: Hello, I’m James Jacobson, founder of Dog Podcast Network, and your host for today’s deep dive into Palladia, a drug that our guest veterinary oncologist, Dr. Megan Duffy, knows a lot about.
Megan Duffy, thank you so much for being with us again.
>> Dr. Megan Duffy: Oh, thank you for having me. It’s always a pleasure.
>> James Jacobson: This is, I think, your third time on Dog Cancer Answers.
>> Dr. Megan Duffy: Yep.
>> James Jacobson: So thank you. You are an important member of our DogCancer.com team. And today we want to talk about Palladia and sort of do a deep dive into Palladia. That is something that we did when Palladia first came [00:01:00] out and was available, but that was over a dozen years ago. More, yeah, it was a dozen years ago. And so we’re kind of thinking it’s time for a catch up because so many people are using it and have questions about it.
So thanks for being with us.
>> Dr. Megan Duffy: Absolutely.
>> James Jacobson: So, when we asked if you’d like to talk to us about Palladia, you said, Yes, I’m really interested. Why do you like Palladia?
>> Dr. Megan Duffy: Palladia is one of those kind of weird things that started out as a very, very niche drug that it was specifically labeled for a specific purpose. And then, in the context of learning more about it, it’s had more and more applications and sort of weird ways and now is kind of a go to for all the weird stuff we didn’t have a good way of treating anyway else. So it’s kind of another tool in the toolbox that doesn’t quite fit with, you know, what we think about with more traditional standard chemotherapy options in a way.
>> James Jacobson: Well, what is some of the weird stuff? When do [00:02:00] you use Palladia?
>> Dr. Megan Duffy: So, Palladia, if you really get into it, and if you’re into the technicalities, it’s labeled for the treatment of high grade mast cell tumors in dogs. And getting into that a little bit further, it then becomes a drug that, with some additional research and work, we said, Hey, this works for a variety of different solid tumors, you know, solid tumors, just like what they sound like stuff you can see and feel and hold in your hand.
And that became, you know, some of our carcinomas, some of our neuroendocrine tumors. Now we use it in cats too. It’s, it’s kind of taken off. I mean, it’s not one drug for a million different solutions, but it has a lot of really wide applications. And I think for me, kind of my, my weirdest tumors are the ones where we can say, you know, gosh, there’s no literature on this. There’s no gold standard whatsoever, but mechanistically, maybe this is an option.
And, you know, [00:03:00] sometimes it works out really, really well, and we can look at a patient and say, this dog, you know, came to me with essentially a death sentence, and we got a lot of really good quality time out of this drug and good quality of life for the dog and for the family.
>> James Jacobson: And Palladia is not, it’s not even a chemotherapy drug, right? It’s a drug used to treat cancer, but it’s not chemotherapy. What’s the distinction?
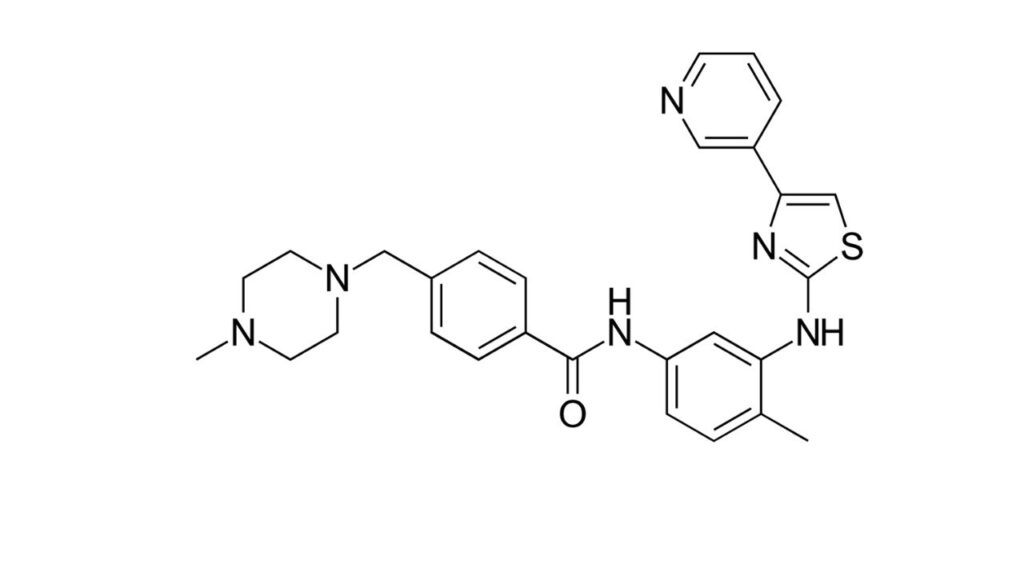
>> Dr. Megan Duffy: In the most technical sense, if you think of a chemotherapy drug as this is a drug that directly kills the cancer cell itself, then Palladia doesn’t fit because most of our chemo drugs are going to interact with how does that cancer cell replicate? It’s going to mess up DNA synthesis or, you know, something in mitosis for the most part. And Palladia instead, one of its main mechanisms is it blocks a lot of the signaling molecules that exist on the surface of the cancer cell that are just waiting for a [00:04:00] reason for something in the environment to tell them it’s time to divide.
And so if they’re not getting these growth signals and these, you know, recommendations to do bad things, they kind of starve to death. And the other way that Palladia works is that it will block some of the tumor cell’s ability to make new blood vessels, so it’s an antiangiogenic drug. And that combination means that we’re sort of selectively starving, there are some immune modulating ways that Palladia also kind of helps the dog’s own immune system fight cancer.
So it’s an indirect cancer cell killing, but still very much an anti-cancer drug.
>> James Jacobson: And it’s one of these drugs that you don’t actually, it’s not injectable, it’s something that you can actually take at home.
>> Dr. Megan Duffy: Mm hmm. And that really opens up cancer treatment to maybe patients that are not the best fit for IV chemotherapy treatment, whether that’s, you know, just getting to a clinic that can give the medication [00:05:00] or stress in hospital, you’re thinking about every nervous dog or fractious cat, something like that, the drive, everything associated with it versus saying, Hey, this is something I can do at home.
And it also, you know, as pet owners, it gives us some control to say, I gave the chemo today. I’m in charge here. I am doing this. So sometimes that’s kind of empowering too.
>> James Jacobson: Yeah, you’re dispensing it. Well, let’s talk about that. So what’s a common dosage in terms of how regularly should when you normally prescribe it? How regularly does someone give Palladia to their pet?
>> Dr. Megan Duffy: So Palladia is not an everyday medication. It’s gonna be given every other day or Monday Wednesday and Friday. For me, most of the time, it’s a lot easier to remember Monday, Wednesday, Friday, so that’s the dosing that we usually use. The nice part of that is, gosh, it’s a pretty low commitment, all things considered, but it needs to be given chronically.
So it’s that low chronic dosing versus [00:06:00] giving a really high dose of an injectable chemotherapy drug every couple of weeks. So it sort of flips that script.
>> James Jacobson: And for how long do you normally give a dog Palladia?
>> Dr. Megan Duffy: Oh, that’s a million dollar question. If you do a deep dive into what’s been published, there’s no clear consensus on when we should stop Palladia. So if it’s tolerated, if it’s affordable, do we give it until the end of time or for as long as it works? And sometimes we do, especially if, if I’ve got a dog with really bad disease and I’m holding it at bay with Palladia, I’m not going to quit. If it’s more of presumed microscopic, there might be something there, then we all kind of debate, do we do six months of Palladia?
Do we do a year of Palladia? What’s our stopping point? And that’s really not well defined, to be totally honest. It’s, it’s sort of a little bit of what makes sense for this individual.
>> James Jacobson: [00:07:00] Okay, and you said if it’s well tolerated and if it’s affordable, we’ll get to well tolerated in a minute because we have so many questions from members of our Dog Cancer Support group and they have lots of questions. They’re very excited to ask them to you and so I’ll ask them others in a bit. But in terms of affordability, and I know things range because you’re in Minnesota and you know We’re in Hawaii and we have people literally all over the world. But how affordable is Palladia?
>> Dr. Megan Duffy: As far as that goes, there’s definitely a big variability that has to do with pet size, unfortunately. I mean, the bigger the dog, the more drug you take. And we’re talking about tablets that you can’t split, break, crush, et cetera. So it’s a combination of how many of this milligram and how many of that milligram and what makes this dog’s perfect dose.
And then that can range a lot. If you’re a teeny tiny dog and it’s $300 a month for the medication, that’s one thing. And if you’re a Rottweiler and it’s over a thousand dollars a month for the medication, that’s sometimes another. [00:08:00] So it varies a lot. And then the other part of that is of course, that’s for the drug itself. Then we’ve got to make sure that it’s, you know, not causing side effects, not harming, and also that it’s working. So then a lot of monitoring comes into play cost wise, too.
>> James Jacobson: So have you seen Palladia cure cancer in some of your patients?
>> Dr. Megan Duffy: Cure is always a tough one.
>> James Jacobson: Right.
>> Dr. Megan Duffy: You know, really, truly, does that mean the dog is in remission and eventually passes away from something else? You know, I, I don’t want to think about my patients getting hit by a bus, but it’s possible. And I’ve, I’ve definitely seen dogs in remission, not die of their cancer kind of best case scenario. A lot of the time I use it for those really awful, gnarly, end stage appearing diseases that don’t become end stage very fast because of the drug, presumably.
So even if I can get a long time with things not getting worse or getting better but not totally going away, I’m really happy with that too.
>> James Jacobson: So [00:09:00] if you do, you know, the most important thing, which we talk about a lot at Dog Cancer Answers is you do surgery and then you add Palladia to the mix. Do you see, you know, a decrease in metastasis?
>> Dr. Megan Duffy: Definitely. You know, not everybody responds to every drug, but the response rate in the right situation is maybe without surgery, was I going to see this again within a couple of months and instead I’ve got a dog who’s a year out feeling great with no obvious disease. I mean that’s a huge win.
>> James Jacobson: So it was approved originally for mast cells and you say you, you know, you try it for all these gnarly things. Is that considered off label or is that just, like, how do you and how do veterinarian oncologists decide, you know, which type of cancer other than mast cell it’s appropriate for?
>> Dr. Megan Duffy: That’s a really good question. And there are certain drugs that due to the way that they are labeled or initially labeled, we can only use them for that specific purpose. I know when Tanovea, you know, first [00:10:00] came out and I believe it’s still the case that it has to be used for lymphoma. It has to be used in a certain way. We can’t just combine it with other things willy nilly. Kinavet, which was masitinib, kind of a sister drug to Palladia, was very specifically labeled. And because Palladia’s initial label is different, but says, Hey, high grade mast cell tumors, nobody’s going to necessarily spend the time, the money, the testing to expand that labeling.
But because most of our cancer drugs, most of our chemotherapy drugs, I mean, those are all used off-label, but have research to back them up that it’ll probably stay in that place where it’s legal. It’s acceptable It’s appropriate to use Palladia in other ways But the label is probably never going to change to show that.
>> James Jacobson: Is that because Palladia came out first? And this was sort of the first time the FDA had approved an oral cancer drug in the veterinary field. And then they labeled it [00:11:00] differently than some of the other ones that came out after that?
>> Dr. Megan Duffy: There’s a lot in terms of labeling and regulatory medicine that it’s going to go beyond the scope of what I know.
>> James Jacobson: Okay. Okay. But it was, it was the first one. Yeah.
>> Dr. Megan Duffy: Yeah. Really, as a, you know, as a targeted oral anti-cancer drug beyond what we had in terms of more metronomic chemo options. You know, it was really a pioneer in very specific targeted treatment for dogs with cancer.
>> James Jacobson: So you’re an oncologist, but is it being used in any things other than cancer?
>> Dr. Megan Duffy: As far as I know, I don’t believe so, but I could very well be wrong if somebody is out there using it for something completely different.
>> James Jacobson: This is a good time to take a quick break and tell you about the website that sponsors this podcast. It’s DogCancer.com. Our guest today, Dr. Megan Duffy, is one of the many medical reviewers and writers on the site.
Every article is researched by and penned by [00:12:00] people with medical knowledge, either veterinarians or veterinary oncologists or cancer researchers with lots of PhDs in their relevant subject areas. Then our science writers ensure that the articles read well and are useful to lay people like you and me.
Finally, each article is medically reviewed to make sure that it is 100 percent accurate. The mission of the site is to deliver you better information today, so you have no regrets tomorrow. Now, DogCancer.com is a relatively new site. It’s only been up several months, but already medical professionals and veterinarians are starting to tell dog lovers who are stunned to learn that the dog has cancer to go to DogCancer.com and to do their research.
Now, sure, you’ll find a lot of information on conventional treatments, but you’ll also find information about other alternative treatments that may help. Things like supplements and dietary changes, and how [00:13:00] things look towards the end of the illness. Everyone involved with DogCancer.com has a lot of letters behind their name, but most importantly, they have love in their hearts, and they all have their own dog stories to tell, just like you and I do. Everyone on the team, what they call Team Dog, all agree with the statement that many things can help treat cancer, not just one or two, and that the quality of a dog’s life and the people who love them, is really important.
If you believe that the future of medicine is integrating everything that we know in a non-dogmatic fashion, and then DogCancer.com is a great resource for you. We hope you’ll check it out. Go to DogCancer.com.
And now let’s go back to our conversation with Dr. Megan Duffy about Palladia. I asked her a little bit about the drugs dosing schedule.
So let’s talk a little bit, you said it’s Monday, Wednesday, Friday, which I think is good because it’s just easy to [00:14:00] remember. But what is the process of, you said you can’t break the capsule, but it’s a pill or a capsule?
>> Dr. Megan Duffy: It’s a tablet. Yep.
>> James Jacobson: Tablet. Okay. So, you know, do you give it with food? What’s the dosing? What does it look like when you administer it?
>> Dr. Megan Duffy: Typically what we want families to do is wear gloves, you know, at least latex or nitrile gloves when they’re handling that medication, especially because as people, we’ve got teeny little absorptive glands on our fingertips. We don’t want anyone microdosing this drug because even when we say it’s not technically chemo, it’s toxic in the wrong circumstances.
So, we’re going to put gloves on, take out the tablets you need. If you’ve got a dog that will take meds in a pill pocket or wrapped in some ham or whatever that looks like, go to town as long as it’s a small amount so we know that the dog took it. It doesn’t have to be given with food, but I always like to, especially knowing when we get into side effects that sometimes we can see some stomach upset.
And if you’ve got at least a little snack on board, that’s [00:15:00] going to go better, but bioavailability absorption.
>> James Jacobson: Everything goes better with a little ham.
>> Dr. Megan Duffy: Oh, absolutely. So, doesn’t change anything. If we gave a dose on an empty stomach versus not in terms of absorption. But, otherwise, you know, it can be something where I’m going to give it Monday, Wednesday, Friday with breakfast or with dinner or with snack or whenever is going to be reasonably consistent.
>> James Jacobson: Okay, so I know the rubber gloves is one of the things that, you know, people are concerned about when they hear about Palladia. Discuss that a little bit more and would it be appropriate for all people, you know, a pregnant woman, for example, to administer Palladia that way?
>> Dr. Megan Duffy: That’s a really good question and thinking about, you know, where do our cancer drugs shine? Well, gosh, we’re going after rapidly dividing cells. And someone who’s pregnant is working on growing some rapidly dividing cells that are good instead of bad, but we don’t want to impair that. So, you know, especially [00:16:00] if pregnant women are in the house, maybe they’re not the best one to be handling the drug.
And if they have to, then it’s definitely the gloves, washing your hands afterwards, being really safe and careful. And similarly too, you know, if I have somebody who is immunocompromised, if they’re recovering from a major surgery, because then there’s that wound healing issue, again, rapidly dividing cells that we just have to be really safe.
And that also extends to, you know, kids who are still growing and developing, for so many reasons, they shouldn’t be the ones giving the dog the Palladia either.
>> James Jacobson: Okay, so that’s going into the dog. What about on the other side when it comes out? Because we all, we all love to pick up our dog’s poop, but is the poop, you know, should that also be treated differently?
>> Dr. Megan Duffy: You know, one of the things we think about in any kind of cancer treatment is what goes in must come out. And, you know, Palladia is just like anything else. It’s going to be metabolized. It’s going to be broken down by [00:17:00] the body, but we know that trace amounts are going to come out. And I consider urine and feces potentially contaminated for just about anything.
>> James Jacobson: Okay.
>> Dr. Megan Duffy: Palladia, you could argue, probably a little bit more is going to come out in poop than pee, but it means if your dog is doing their business outside, hey, that’s half the battle, right? That it’s going to go out hopefully in grass, soil, so that soil contact, direct sun exposure, extreme heat or extreme cold, time, that’s going to help break down some of those trace amounts. But it also means we’ve got to be normal people who are not picking up poop with our bare hands.
>> James Jacobson: Okay.
>> Dr. Megan Duffy: And that seems reasonable when you say, yeah, I’ve got my scooper. I’ve got my bag. If we’ve got a three year old running around the backyard, it means we got to scoop before anybody accidentally steps in something, touches something, et cetera, because there’s that unknown.
Then it also means. Hey, if we’re having a rough day and the dog went potty in the house or had an accident in their bed, then it means [00:18:00] we’ve got to clean up those hard surfaces with gloves on. Dawn dish soap actually does a really good job of deactivating any kind of trace chemo or anti-cancer drug molecules.
And then all that soft stuff, you know, the bedding, et cetera, we’re going to toss that in the washer by itself. It’s going to be double washed on two hot water cycles and then we’re going to be pretty darn good to go as far as contamination. But the other stuff, just like any other drug, dogs can sit on your lap, you know, they can hang out with you.
They can be petted. They can interact with their other housemates, you know, dog, cat, human and otherwise. Share dishes and bedding, and that’s okay. You know, if there’s a drug that. It puts you on lockdown because you’re on something that’s hazardous to everyone around you. That’s a quality of life issue.
>> James Jacobson: Right.
>> Dr. Megan Duffy: That’s not, that’s not appropriate.
>> James Jacobson: Okay. What about, I don’t know, doggie kisses?
>> Dr. Megan Duffy: That is, it’s kind of debatable and arguable amongst even oncologists where, uh, depending on how [00:19:00] easily they swallow it, could there be trace Palladia on the dog’s tongue way in the back? So I’d say to be safe, probably that first hour or two after the dog takes a pill is probably not the best time to have them lick your entire face.
But on a normal kind of everyday, the dog licked me situation, I feel like that’s reasonable and that’s okay.
>> James Jacobson: Okay, so we just don’t leave any bodily fluid undone here. I’m assuming vomit would also be a problem in the same classes. That species. Yeah.
>> Dr. Megan Duffy: Yeah. Let’s throw some gloves on, clean it up as best you can, go about your day. You know, that’s kind of the nature of the beast, but just kind of treating everything as a potential risk, but also not putting the dog in a bubble for the rest of its life. So a little bit of, you know, keeping that balance.
>> James Jacobson: Great. And you say when it’s well tolerated, a dog can be on it for the rest of their lives. What does that mean in terms of visits to you? How frequently do you want to see a [00:20:00] dog that’s on Palladia and what kind of tests do you run?
>> Dr. Megan Duffy: That’s a really good question. And especially when we’re thinking about what side effects can we see and what do I need to screen for too? You know, the dog is going to tell us if they’re having stomach upset, you know, if they’re not eating well, if they’re nauseated at home, if they’re vomiting, having diarrhea.
But the other things that I need to make sure I’m watching for are are white blood cell counts in a safe range? Are platelets falling low? Are we losing protein? And sometimes we can see protein loss through the kidneys or increased blood pressure, you know, changes like liver and kidney value changes.
So a lot of this is going to be monitoring blood work. And then occasionally we’re going to check urine. We might check the blood pressure, and that might look like a every few weeks at first or often, you know, once a month as kind of a long term maintenance plan. Maybe we do some of those other tests more often or less often, depending on what kind of values the dog started with.
[00:21:00] And then over time, if it’s a good fit, then maybe we’re saying, well, gosh, we could do this every six to eight weeks or every two to three months. So sometimes, again, with that well tolerated being the underlying theme that we can say, all right, this is going really, really well. We’re not going to stop looking, but we’re going to space things out a little bit.
>> James Jacobson: Got it.
>> Dr. Megan Duffy: And the other part of that, of course, is if I’m using a drug and it’s well tolerated, that’s half the battle, but it’s also got to work. And so depending on the disease, that’s going to at least mean physical exam. We may be doing, you know, x-rays, ultrasound, some kind of imaging to say, Hey, has this disease spread? Has it gotten bigger? Where are we at? All those sorts of things.
>> James Jacobson: Okay. So, as I said, our listeners and our participants on our Dog Cancer Support group have tons of questions. And a lot of these have to do with the side effects associated with Palladia. And so, if you’re going to see a side effect, what are the [00:22:00] common ones and how soon do they start?
>> Dr. Megan Duffy: That’s a perfect question. And most common side effects for me are going to be those kind of gastrointestinal things like stomach upset. So a dog who’s not eating very well, if they’re showing me signs of nausea, like drooling, licking lips, swallowing hard, maybe walking right up to the bowl with interest and then kind of not quite being able to eat, or somebody who truly is vomiting or having diarrhea, especially really sudden onset liquid diarrhea.
And for the most part, if I’m going to see a side effect like that, it typically is going to come on within the first two weeks or so, often to the tune where if we start this drug, I’ll often send home, you know, a two week trial course.
Is this a good fit? Before we order a ton of medication or send you home a huge bottle of it, is this going to be tolerable because there are those dogs that are really sensitive and even at lower doses or different intervals, Palladia is just not the right [00:23:00] fit.
>> James Jacobson: What percentage of dogs do you end up saying, you know, this is not a good fit with?
>> Dr. Megan Duffy: For me, that’s pretty low and some of that is chatting through, does this make sense? Is this a dog with a really sensitive stomach or a history of other problems? So I would say less than 5 percent of the time we have to say, gosh, this is just not going to work for you, but it’s a risk and it’s worth talking about and kind of sorting out upfront as much as we can.
>> James Jacobson: And then that lack of appetite that a dog sometimes experiences that also a really, I mean, it’s one of the more common one, but it’s not that frequent.
>> Dr. Megan Duffy: As far as that goes any of those gastrointestinal signs, I would see that in maybe 20 percent of dogs on Palladia
>> James Jacobson: Okay. So do you then do something to like enhance their appetite or do you just continue, or give them like Pepsid AC, or something else?
>> Dr. Megan Duffy: A lot of the time depending on the dog it may be, do they need, you know, a chronic antacid? Do they need Pepcid? Do they need Prilosec? And some dogs [00:24:00] do. Some of our mast cell tumor patients are already on them, you know, for tumor related reasons, and then occasionally if they’re just a little herpy after that dose of Palladia, do we become more proactive and we do a nausea medication like Cerenia an hour before the Palladia is given to kind of help settle the stomach.
And of course we’ve got much better appetite stimulants than we used to and all of those things. Some of it boils down to, to say, if you can only tolerate Palladia because you’re on four other drugs to deal with how your pet feels, that’s probably not a great fit. You know, we can struggle through it, but it becomes, are we making this dog a walking pharmacy just to get through this drug?
So it is kind of a slippery slope of, hey, you need a little bit of help here and there, no big deal, but If we’re really forcing it, again, it may be not the right fit.
>> James Jacobson: But you don’t see that often in your patients?
>> Dr. Megan Duffy: I really don’t.
>> James Jacobson: Is that a function of the way you’re, [00:25:00] like, really assessing whether this is a good candidate for Palladia based on, you know, what else you know about the dog, or is it just, like, genetics?
>> Dr. Megan Duffy: I think a lot of it is that upfront conversation. You know, if I have a family say very directly, their dog has a sensitive stomach, they have a history of doing poorly with certain medications. Maybe this isn’t the right choice. Then we weed out some of them. The other part, which I think is really interesting and goes along with Palladia’s history is if you really dig through the labeled dose and the dose that Palladia was started at, it’s a much higher dose than any oncologist is really currently using.
And part of that was the maximally tolerated dose at MTD is, is what we use for all of our chemo drugs, right? Like what is the highest dose we can give that’s going to be effective without causing major issues. And the MTD of Palladia is not the biologically effective dose. That’s actually a little bit lower.
So [00:26:00] side effects like stomach upset were as much as 40 percent at that maximally tolerated dose. But now that we’re using kind of a more widely accepted kind of biologically effective dose, I’m also seeing fewer side effects. So it just fits better that this is more tolerable. It still works really well. Kind of like everybody wins.
>> James Jacobson: So you’re using lower doses well outside of our favorite MTD that we talked about a lot, which is this like how much would it take to just basically get the dog to die and then we’ll teeter off of that and then we’ll know that’s the max So it was labeled for a really high dosing but you’re able to use less because you guys have had a dozen or more years of experience with it.
>> Dr. Megan Duffy: Mm hmm.
>> James Jacobson: Okay, and it’s just as effective as at the high dose
>> Dr. Megan Duffy: Absolutely, there were kind of rumblings about that for a long time and then some more in depth surveys of oncologists and we said, well we’ve all kind of independently come to this conclusion that lower doses seem to be better [00:27:00] in terms of tolerability without changing outcome.
>> James Jacobson: That’s great that you’ve all collectively discovered that a lower dose actually works as well as a higher dose and has fewer side effects.
Let’s take a quick break right here to hear from our sponsor. And we’ll be right back because I have a question about how oncologists all talk about these things
And we’re back with Dr. Megan Duffy. Before the break we spoke a little bit about how you and your colleagues all talk about the dosing and how it doesn’t necessarily need to be as high as was originally thought So how do those conversations go? I’m just kind of like, you know, is this something you guys are sitting around over a glass of wine at a oncology conference? Or how do those conversations go where you guys are saying, well, this is what I’m experiencing in clinic.
>> Dr. Megan Duffy: I think a lot of things start like that where you know we’ll kind of get together and say, you know, how have you been using this drug, or has it been working well for you? I’m [00:28:00] really having a problem with these side effects and you know, somebody will say I’m using a bit of a lower dose and it seems to be better tolerated, or so and so has been trying this dose and here’s what they find, and when enough people talk about it enough then it becomes, you know, surveys coming out at our cancer meetings or studies saying, well, gosh, these people are using this dosage and their results are just as good and their side effects are lower.
So it’s in a way nice to be sort of a small community and a really connected community in the veterinary oncology world because we can have those little conversations kind of make big ripples.
>> James Jacobson: Yeah. And it is uber small. How many oncologists are there right now in North America who are practicing, not like, you know, in the lab, but, but practicing like you are?
>> Dr. Megan Duffy: Oh, I wouldn’t know, but it’s hundreds.
>> James Jacobson: Hundreds, yes. Hundreds. Okay. And is, do you know, is Palladia used outside the United States as well?
>> Dr. Megan Duffy: It is.
>> James Jacobson: Okay. So a lot of people and basically so the trend is lower dosages [00:29:00] are doing just as well and you’re seeing obviously less side effects with the lower dosages. So again, because people are so concerned about side effects, do side effects stop if you stop taking Palladia?
>> Dr. Megan Duffy: Oh, definitely. You know, sometimes we’ll have to take that drug holiday and say, okay, your dog is having diarrhea. This is not what we want. Stop the Palladia for a week. Let’s get the diarrhea under control. Let’s restart at a lower dose or a different dosing interval and see if that’s a better fit. And if it’s not, and if we really have to push through, if we stop Palladia, we can get that dog back to normal again.
It’s not a side effect that we’re going to have for the rest of the dog’s life or something like that. So that’s the good part is they will go away.
>> James Jacobson: So again, and I think we may have covered this, but I want to kind of be comprehensive. One of the questions we get are like, when do you see fewer and when do you see more side effects? Like, is there a rule of thumb that you look [00:30:00] at to determine that ahead of time?
>> Dr. Megan Duffy: As far as that goes, I, I think a lot of it is, is more individual. Dogs that already have issues that could be made worse with Palladia are probably going, you know, to be the ones that may have more side effects or that we may have to make changes for. Again, those dogs with really sensitive stomachs, they may be the ones that are going to, you know, look at a tablet and throw up almost it seems like, and we say, that may not be the right drug for you.
>> James Jacobson: And some people are asking if their dog has heart disease or liver disease or kidney problems, is Palladia appropriate?
>> Dr. Megan Duffy: Definitely, depending on the individual. We can see things like, you know, protein loss through the kidneys. If you’ve already got kidney disease and you’re already struggling with how much protein is being lost into your urine, we could make that worse.
And it means it’s not a no, but it’s, you know, it’s a yes, but. We’ve got to really watch carefully. If we’re seeing things get worse, we’ve got [00:31:00] to take action. And it might be something where we say, gosh, your dog’s kidney disease is getting worse. I don’t know if Palladia is worth it. Or if your mild liver disease becomes moderate liver disease, is that something I can manage because Palladia is doing something that’s really, really useful and worthwhile.
So definitely a balancing act where I wouldn’t immediately say, nope, you have one abnormal value, you can’t have Palladia, but what makes sense for this individual.
>> James Jacobson: Well, are there any cases where you would just say, no, we’re just not going to use Palladia? When you’re dealing with one of these, you know, crazy gnarly tumors, and you look at something and you’re like, it’s going to basically disqualify this dog from using Palladia.
>> Dr. Megan Duffy: I think if we have other diseases that are so severe. that Palladia would just push this dog over the edge. You know, if you’re already an end stage kidney failure, if you have very limited liver function, if your bone marrow is such a disaster that, you know, a gentle breeze is going to be a [00:32:00] problem, then Palladia is not worth the risk.
>> James Jacobson: Okay, and what about using Palladia with other chemotherapy or even radiation?
>> Dr. Megan Duffy: That’s really interesting too, because there’s been a lot of research in terms of what’s the best timing of Palladia? Is it after traditional chemo? Is it with traditional chemo? And especially from a chemotherapy standpoint, Palladia can double down on side effects if we give it with chemo and we’re not making dosing adjustments.
And that’s, that’s kind of its own drug dependent dance of we could make white blood cell counts worse, we could make stomach upset worse, those sorts of things, so it’s still very much debatable and the literature changes a lot from even year to year of no, we shouldn’t give these drugs together, no we can but we can change these doses in order to do it and maybe these outcomes are better, no no no if we do it this way the outcomes are better, so there’s that piece that I think is still being fine tuned, and then radiation [00:33:00] wise.
>> James Jacobson: Well, what’s your personal experience? Do you personally use chemo at the same time?
>> Dr. Megan Duffy: I don’t typically use traditional chemotherapy and Palladia together, in terms of the side effects that I’ve seen, you know, the cost issue becoming a factor, and knowing, quite honestly, we have a limited amount of drugs. If I can space them out and use one at a time, sometimes that gives me more time with tumor control.
That been said with low dose oral chemo with our metronomic chemotherapy drugs, they sometimes can combine fairly well with Palladia and potentially that gives us a little bit more of that immune modulating effect that helps the dog’s own immune system kind of seek out and destroy cancer cells. So there’s a little bit of information about Palladia and metronomics.
>> James Jacobson: Which metronomics would you use?
>> Dr. Megan Duffy: I use Chlorambucil more than anything else because of its pretty limited side effect profile. I’ve also used Palladia with Cytoxan or Cyclophosphamide as [00:34:00] well.
>> James Jacobson: Okay. And then I interrupted you and you were going to get into radiation. What about radiation and Palladia?
>> Dr. Megan Duffy: So Palladia may actually have some function as a radiation sensitizer and that’s still kind of being looked at but it also means if I’m treating a dog where Hey, radiation could help. Palladia could help, especially if we’re not using really, you know, intense radiation protocols where sometimes radiosensitizers are good and bad and they can help with side effects too. But there’s definitely a role for certain patients where maybe we do both at the same time.
>> James Jacobson: And just to be clear, a sensitizer increases the sensitivity of the patient to the radiation or the chemotherapy in the case of chemosensitizer. Okay. So you generally don’t want to use, I mean, radiation is still rather not that common with dog cancer, but you don’t use it, or it sounds like something that you’re not using with Palladia.
>> Dr. Megan Duffy: I’d say the, the best application is, [00:35:00] is some of those really big, ugly, non resectable mast cell tumors that maybe we start Palladia, we send them for radiation, we keep them on Palladia while they’re getting their radiation and then afterwards to, or even some really, you know, nasty oral tumors or something like that where I start the Palladia. I send them off for radiation They come back still on it because we need all the help we can get.
>> James Jacobson: Got it. What meds, if any, would you not want to continue using when a dog is on Palladia?
>> Dr. Megan Duffy: As far as that goes there, there is a role for saying gosh if I have a dog on other immune suppressives of any kind, we really don’t want to double down on that. And that could be dogs on immune suppressants because they have really bad allergies. They have immune-mediated skin disease, immune-mediated, you know, anemias, or thrombocytopenias where if we’re already suppressing part of your system and we could potentially double down, [00:36:00] that’s not ideal.
>> James Jacobson: Okay. And dietary restrictions? Are there any dietary restrictions when, when a dog is on Palladia and it’s being, you know, tolerated?
>> Dr. Megan Duffy: Not necessarily, at least in my patients, they eat their usual diet, including their snacks and their cookies and everything else. So, I, I don’t typically worry about diet restrictions for them.
>> James Jacobson: So, if someone is, you know, after having heard all of this, still has questions, what are the questions that they should discuss with their veterinarian about Palladia? If you, I didn’t know as much as you did, but you had a good grounding in this and you had to take your dog in for treatment. What are the questions that you might ask?
>> Dr. Megan Duffy: I think it’s always worth asking, Is Palladia a good choice for my dog? Does it work for my dog’s cancer? Is it the best choice for my dog’s cancer? Are there other things that I should also be thinking about? And is my dog specifically at risk [00:37:00] for side effects based on other concurrent diseases or concurrent medications? Those would be a lot of my questions, you know, if I was going into this saying, Is this appropriate? Is it the best use for this, you know, situation?
What’s been your success rate in similar patients? Just to get an idea of, of that sort of comfort level.
>> James Jacobson: Okay, so now I’m going to ask you to polish your crystal ball. So, I mean, Palladia’s been out, as I said, a dozen or so years. It’s one of these anti-cancer meds. We’ve seen a couple of others. What do you think is the future for these types of take at home anti-cancer meds in terms of treating dog cancer or pet cancer in general?
>> Dr. Megan Duffy: You know, it’s, it’s always a win win. You can take it home, it’s oral, it’s easy, it’s low stress. And the really neat thing about so many ways of how Palladia works is it’s a lot more targeted than just generalized killing [00:38:00] rapidly dividing cells when we’re specifically looking at signaling pathways and growth factors and it’s getting a little bit more targeted.
And I’d love to see that trend continue where we have very specific targets and mutations in tumor cells that we can address with oral therapy at home and have things be a little bit more personalized. It kind of also is stepping over that threshold of really individualized medicine. You know, what is, what does this tumor have that maybe other tumors don’t? What are our, you know, druggable targets, so to speak, that specifically we can inhibit with our medications?
>> James Jacobson: Do you see drugs in the pipeline that are going to do that the same way as Palladia has?
>> Dr. Megan Duffy: I think the potential is there, and there are definitely several private companies that are working on the other piece, which is sequencing the DNA of your dog’s tumor, finding those mutations, and then saying, do we even have a drug that works against these [00:39:00] mutations? What’s the safety? What’s the efficacy? So there’s a lot of, there’s a lot of gaps that we still need to bridge, but I think it is eventually coming. I think in a way that is the eventual future of veterinary oncology.
>> James Jacobson: Well, that’s probably for another episode of Dog Cancer Answers. We’ve actually covered that in the past, but are you like kind of looking at that with your own patients? Where you’re sequencing the DNA and looking for drugs that are specific?
>> Dr. Megan Duffy: It’s something that I’ve used with just a couple of patients, but it’s labor intensive, it’s time intensive. It costs a lot of money and it’s got to be for the right situation. And I think as that process gets a bit more streamlined and as we get better drugs to do something with, you know, it’s, it’s hard to get a report back and say there’s 50 mutations and we have drugs for none of them. So I think it will come. We’re not there yet. That’s for sure.
>> James Jacobson: So we have the data on the DNA, we just don’t necessarily have the drugs for what the genetics is revealing. Wow. Well, we will have you on [00:40:00] another episode when there’s more information about that, but I want to thank you so much for your time today, because Palladia, It’s long overdue that we’ve done an episode on Palladia. Any last thoughts about Palladia?
>> Dr. Megan Duffy: I’d say as far as that goes, you know, I would consider Palladia, especially when we don’t have obvious options or other good options. And, you know, if you are a person dealing with cancer in your own dog, it’s always worth asking your veterinarian if this is going to be an option.
>> James Jacobson: Megan Duffy, thank you so much for being with us today.
>> Dr. Megan Duffy: Thank you. It’s always a pleasure.
>> James Jacobson: And thank you, listener. Please check the show notes for links to articles about Palladia and other relevant links on DogCancer.com. Also, don’t forget to subscribe to this podcast and join our Facebook support group at DogCancer.com/support.
I’m James Jacobson, and from all of us here at Dog Podcast Network, I’m wishing you and your dog a very warm [00:41:00] aloha.
>> Announcer: Thank you for listening to Dog Cancer Answers. If you’d like to connect, please visit our website at DogCancer.com or call our listener line at (808) 868-3200. And here’s a friendly reminder that you probably already know, this podcast is provided for informational and educational purposes only. It’s not meant to take the place of the advice you receive from your dog’s veterinarian.
Only veterinarians who examine your dog can give you veterinary advice or diagnose your dog’s medical condition. Your reliance on the information you hear on this podcast is solely at your own risk. If your dog has a specific health problem, contact your veterinarian. Also, please keep in mind that veterinary information can change rapidly, therefore, some information may be out of date.
Dog Cancer Answers is a presentation of Maui Media in association with Dog Podcast Network.