EPISODE 228 | RELEASED September 18, 2023
Repurposed Drugs for Cancer (Mast Cell Tumors) in Dogs | Dr. Lauren Barrow
Tracie is thinking her dog’s mast cell tumor might benefit from Panacur (fenbendazole). Are there any other repurposed drugs she might consider?
SHOW NOTES
It’s so exciting when a familiar drug in one area shows promise as a new treatment for another health problem. Researchers and clinicians pay attention, especially when the drug is inexpensive and easily tolerated.
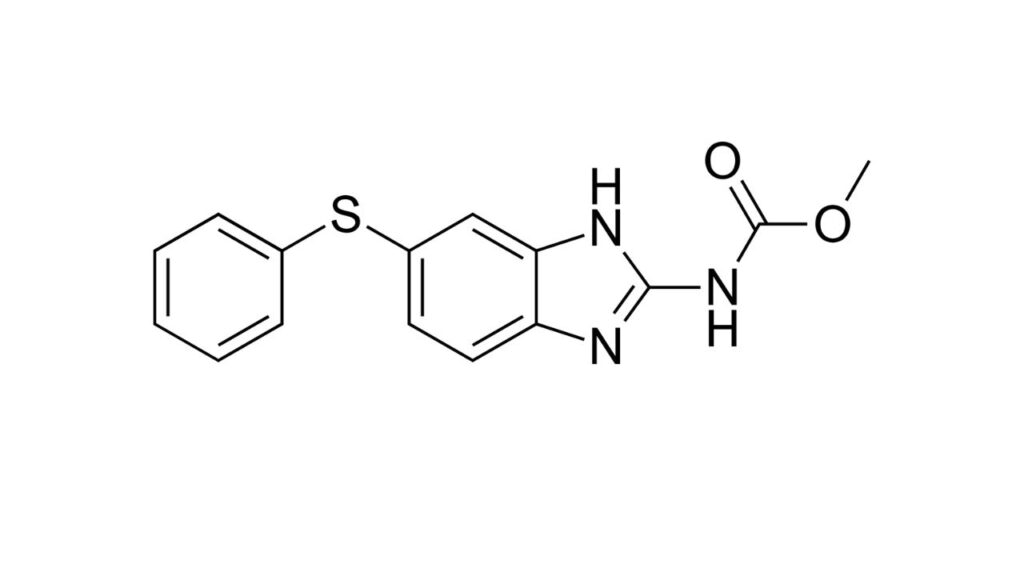
Such is the case with Panacur (fenbendazole), a dewormer that has caught the attention of cancer researchers. It’s early days of studying its effects on cancer, but some people want to start using it now!
And no wonder. It’s mechanism of action is the same one used by several well-known cancer drugs! But would the high doses needed cause the same severe long-term effects of other chemo drugs we’re already using?
Dr. Lauren Barrow joins us for a fascinating discussion prompted by listener Tracie’s question about her dog’s mast cell tumors. We talk about the thinking general practitioners engage in around repurposing drugs for cancer … and why a trip to the oncologist might be a good idea.
After all, oncologists (especially veterinary oncologists) are not just the keepers of insights and expertise about standard treatment methods … they are the researchers on the cutting edge of oncology. They’re the ones who research and repurpose drugs!
>> Dr. Lauren Barrow: From a general practice point of view, when I find a mast cell tumor, I will often prescribe Benadryl, that’s because it’s an antihistamine, and I am not doing that because I think it’s going to cure the tumor or make the tumor go away, but I’m trying to cut back on the side effects of that tumor.
>> Announcer: Welcome to Dog Cancer Answers, where we help you help your dog with cancer.
>> Molly Jacobson: Hello friend, I’m Molly Jacobson, and thanks for joining us today. Today we’re taking a listener line call from Tracie, whose dog has mast cell tumor, and her question about using a dewormer to treat it led to a broader discussion about repurposed drugs and their use in dog cancer.
Joining us to answer Tracie’s questions is Dr. Lauren Barrow, Dr. Barrow. Thanks so much for joining us again on Dog Cancer Answers.
>> Dr. Lauren Barrow: Thank you for having me.
>> Molly Jacobson: So let’s listen to Tracie’s call and see what your thoughts are.
>> Tracie: Hi, my name is Tracie and I’m calling from Las Vegas. I just recently got my eight year old dog neutered and about a week after neutering him, the vet calls me and they found a growth in the area and it came back as an MCT stage 3 tumor. I was wondering if, because we don’t want to do the chemotherapy and radiation as the vet recommended. She wants us to take the dog to an oncologist, but we just don’t think that’s any quality of life.
Now, the doctor said that when he removed the tumor, he cleared the margin. And it didn’t look like it spread, but there’s a very high chance that it can metastasize. And I was wondering if there was any repurpose drugs out there. I heard of Panacur and I just listened to a podcast on that. I’m looking to Dr. Nancy’s opinion, but I was wondering if there is anything else out there that could help my dog. He’s very healthy and it’s his normal self now. So please help or give any advice. Thank you.
>> Molly Jacobson: So Dr. Barrow, Tracie is wondering, and I think like many people, it sounds like she might be a little hesitant about chemotherapy and about radiation, and a lot of people feel that way they worry about chemotherapy being something very dramatic and drastic the way it is in humans. And so she’s wondering about any other drugs that might be a little bit, I think she’s hoping more friendly and having fewer side effects. So there’s a lot here to unpack.
I guess the first question we should answer is having listened to the other show with Dr. Nancy, we’ll have a link to that in the show notes about Panacur, is Panacur good for mast cell tumors?
>> Dr. Lauren Barrow: So Panacur, if you’re not familiar, is a dewormer and I use it all the time for certain kinds of gastrointestinal parasites. And we give it for a few days at a time in a normal recommended dose and it works great on the little wormies. So, I’m not completely sure why it’s been on the news lately. I went looking a little bit about why because I’ve had a couple people ask me too about it. Because mast cell tumors are one of the most common tumors that I come across in general practice.
So, I’m not sure why Panacur is popping up right now. I think there was a study. What I could find, and correct me if you know anymore, but what I could find was a study, it was a few years ago actually, that had some mixed results that maybe it was inhibiting some tumor growth in a Petri dish, and I think it was mouse lymphoma specifically. And so mixed results and maybe, maybe it helped a little bit in the Petri dish. Maybe it worked better if there was vitamins added.
What can you add to a Petri dish to make a tumor stop growing? You could add all kinds of stuff probably to a Petri dish to make tumors stop growing. The other thing that caught my eye was that you have to have a pretty high dose of it for it to make any sort of difference, to the point where maybe the risks are not going to outweigh the benefits, and you would have to give it for a really, really long time in really high doses to even come close to the results of a mouse cell for a different cancer in a dish.
So I don’t personally know anybody who is a veterinarian who is recommending this at this time. Maybe there’s more we need to learn about it. The other thing I noticed is the way that it works is through working with the microtubules, which is a whole lot of science you don’t want right now. But there are a couple other chemotherapy drugs that work in the same fashion.
>> Molly Jacobson: Right.
>> Dr. Lauren Barrow: That we know are available and that we know work and that do have studies to back them up. So that was a whole lot of stuff I said to come back to. I don’t think Panacur will work, so. But ask the oncologist.
>> Molly Jacobson: But ask the oncologist. And it’s so important to understand that there are, yes, many drugs that are repurposed for other uses. Because drugs have more than one action in the body, or they can, sometimes, and that it’s important that the reason Panacur is being investigated sort of slightly in small studies now that maybe is interesting for people to look at further, is actually because it’s behaving the same way that chemotherapy drugs your oncologist might recommend behave, so it’s the same mechanism.
It’s the same actual thing that’s happening in the body. It’s just with a drug that we think of as a dewormer that is very effective and quick at deworming, but might given higher doses and possibly really bad side effects over the long term also have an effect on cancer, but then those side effects might be equivalent to the ones you’re worried about in chemotherapy.
>> Dr. Lauren Barrow: Right.
>> Molly Jacobson: So it’s sort of like six of one half a dozen of another at this point in time We do have good information on DogCancer.com about Panacur So I’m gonna make sure we get those links in the show notes so that you can understand better why it’s Interesting and sort of piqued some interest but why it’s not yet in common use, for sure, and what the real concerns are about toxicity, because it’s good at high doses over a long period of time.
>> Dr. Lauren Barrow: And it’s just not helpful yet, but maybe someday.
>> Molly Jacobson: But maybe someday, because maybe there’s ways to amplify its effects. Maybe there’s ways to mitigate the side effects, like there’s things that they might figure out in the future, right? Like all of these things. Yeah.
>> Dr. Lauren Barrow: Right. We’re figuring out new stuff all the time.
>> Molly Jacobson: Exactly. So her other questions, are there any other repurposed drugs out there that might help? And I’m kind of assuming again, that she’s looking for something that’s not typically used for chemotherapy, but any drug that is used to treat cancer could be called chemotherapy, right?
>> Dr. Lauren Barrow: Right. So to back up with, with mast cell tumors, they’re a tumor of the immune system and it’s a certain type of cell that circulates and releases histamine, which is the same kind of thing, you know, like when you have your allergies and you’re getting all the boogers and stuff, it, histamine reaction, kind of, inflammatory process that these tumors have.
So from a general practice point of view, when I find a mast cell tumor, I will often prescribe Benadryl, that’s because it’s an antihistamine. And I am not doing that because I think it’s going to cure the tumor or make the tumor go away. But I’m trying to cut back on the side effects of that tumor because most of the time what has happened is that the dog came in and they had a mass somewhere and I poked it with a needle to get a sample and then it was really pissed off. You know, we have an angry tumor here now. I know.
>> Molly Jacobson: Can you see that right in the clinic when you’re taking a fine needle aspirate?
>> Dr. Lauren Barrow: Maybe not in real time, like it’s blowing up like a balloon.
>> Molly Jacobson: Okay.
>> Dr. Lauren Barrow: But one thing that will make me go, oh man, is if I poke it with a needle and it bleeds a whole bunch. And you know, if, if I’ve got two tumors on a dog and I poke one and it bleeds a whole bunch and the other one doesn’t, I can almost as I’m walking that slide to the microscope be like, man. So I don’t want that dog to go home and be itchy or have side effects or have some sort of an inflammatory cascade, which is not common, but not impossible, especially just stop by Walmart or whatever and get some Benadryl.
>> Molly Jacobson: So what’s an inflammatory cascade?
>> Dr. Lauren Barrow: So complicated medical stuff, right? We all have immune systems. We all have lots of different parts of our immune system. Some of it is just basic things like I have skin so that the parts underneath don’t get infected. You know, I have mucus so that the germs get caught in the mucus and I can sneeze them or cough them out.
And then there’s also cells that work in our immune system. I’m sure everyone’s heard of T cells and B cells and, you know, all of the immune cells that we have going on. And so there’s a whole army of those. And they have a whole mess of complicated signals that they send to each other and, you know, one of them over here will detect an invader germ and send chemical signals to the other ones and then they go, oh, okay, I’m on it.
And then they’re so it’s like G. I. Joe, there’s sending little signals to each other that we don’t even know is happening. So when that goes awry, either with cancer or, you know, there’s different systems in the body that can just, for whatever reason, get out of whack. You can have an inflammatory avalanche kind of a situation where there’s too much signal, it’s going too far. That’s basically what anaphylaxis would be, right?
>> Molly Jacobson: Oh, okay. All right. So a massive allergic reaction.
>> Dr. Lauren Barrow: Explosion. Yeah.
>> Molly Jacobson: Could be called an inflammatory cascade.
>> Dr. Lauren Barrow: Yeah, a little inflammatory storm, if you will.
>> Molly Jacobson: Okay, sure.
>> Dr. Lauren Barrow: And that’s obviously not a thing that is supposed to happen.
>> Molly Jacobson: Right.
>> Dr. Lauren Barrow: That’s not normal. Your body’s supposed to say, Here’s the bacteria, eat it, kill it, yay. And then they keep doing what they’re supposed to be doing. Not eat it, kill it, freak out through your whole body. You know what I mean? And now it’s just like a disaster, but mast cell tumors are kind of creepy like that sometimes. And grade three, which is what she had mentioned, is pretty serious.
I don’t come across them very often. By far, the majority of them are grade two. And if you, if you get online and start doing the Dr. Google thing, you’ll find that there’s a lot of arguing and back and forth about how reliable is the grading system, which one should we use? Should we biopsy first or take the whole thing?
How wide of margins, which means how much of a chunk should we take out? There’s a lot of back and forth and arguing. So the grade three, I know she said that they got good margins, which is great. And that there’s a high chance that will metastasize. And one thought I had when I was reading that question is that it might be worth it to do some work to see if it’s metastasized now or down the road.
Do some x-rays or ultrasound, things like that to see, but the thing that I thought of the most, which I think you’re probably going to bring up, is the chemotherapy situation. I would definitely recommend going to the oncologist. I think a lot of times the oncologist and the recommendations that they have are not what you think they’re going to be.
It is worth it to me to go have an exam, bring your questions, bring your story, bring your dog, and pick their brain and have them tell you what they think it is, how to check it, and when they come up with, especially mast cell tumors, there’s going to be a lot of different options for chemo, that the oncologist can help you decide what would be cost effective, safe, what would work best for your dog with her particular health history, you know, what all of these trials and tailor that to your dog.
And then if you don’t want to do it, you can say no.
>> Molly Jacobson: Right. Going to an oncologist does not mean you’re going to use chemotherapy.
>> Dr. Lauren Barrow: Right. Right. And so that’s the first thing is at least get the information, at least have the meeting before you decide you don’t want the job. Go to the interview, let’s check it out, let’s see what the deal is, don’t just write it off. You may be pleasantly surprised and I’ve had lots of people that I’ve had this similar discussion with said, I know right now you think you don’t want to do this or that or this. You don’t have to just go get the information, get the actual deal. So I would encourage her to go and check it out.
>> Molly Jacobson: Okay, let’s pause right here for a break to hear from our sponsors. And then when we get back, I want to talk more about what oncologists actually bring to the table, just so Tracie has that perspective.
And we’re back with Dr. Lauren Barrow answering Tracie’s phone call about her dog with mast cell tumors. She said she’s a little shy about chemotherapy and she’s looking for some alternatives. So let’s just talk a little bit about oncologists and what their deal really is. I think people assume that an oncologist wants to push drugs, surgery, and radiation.
And doesn’t consider other things. And I understand that’s a perception that’s out there. It’s just in my almost, I don’t know, 2007 to 2023. So almost, you know, 15 years, I guess, of working with veterinarians. I’ve just never found an oncologist who actually did push these things. I have found them to be very informative.
Also, I have found them to be incredibly interested in quality of life, like really interested in life quality. They don’t want you to come and spend money with them and then be angry because your dog is really sick. So that’s always a priority for them as well. And we often have an assumption that it’s not.
But even someone like Tracie, who is interested in preserving life quality, could still actually benefit from the expertise of an oncologist who could actually be realistic and informative about that specific diagnosis. Am I right? I mean, they just know, I mean, they just know more than a GP in general.
>> Dr. Lauren Barrow: Oh yeah, for sure. And they do. I mean, they started out as regular vets, just like us, and then they kept going to school and training, to learn specifically the bazillion of options out there and chemotherapy in humans. We’ve all seen the movies and the TV shows, and I think almost all of us have known someone by now who has gone through chemo and, and it’s this horrible, bald, sad, sick, nauseous, you know, all of these horrible things.
But keep in mind the goals in human cancer treatment are often a little bit different than in dogs and cats. In people in general, we’re looking for a cure, we’re looking for remission, we’re looking for resumption of your life trajectory. If you’re a kid with cancer, we’re trying to kick that cancer’s rear end so that you can grow up and have a life and be a person where if you’re a, you have a family to raise, you have a job to go to, we’re trying to kick that cancer out.
So, in general, dogs don’t do those things. They don’t, you know what I mean there? We don’t have them long enough anyway. We’re lucky if we get 10, 15 years with our little furry soulmate, we’re not going to make those last couple of years horrible, bald, nauseous, sick, sad. We’re just trying to buy some time and some quality of life at the same time.
They don’t need to go back to a job. They don’t need to raise a family. They just need to be happy with you. And so I think if you look at the goals of a veterinary oncologist, and not to say I don’t know some great human oncologists, for the record, who also are very, very into quality of life, but they are not going in this with different goals from you. And if you’re not sure, you tell them, my goal is quality of life for my dog. And a lot of these medications and chemotherapies and radiation and stuff, actually do help quality of life.
>> Molly Jacobson: Right.
>> Dr. Lauren Barrow: Depends on the type, obviously, but that’s, I think, what you’re saying is that the perception of what they’re gonna offer you is often wrong with people. So, that’s why I say go yourself, ask them. Tell them, this is my dog that I love, what can we do to help her? I don’t want her to be nauseous, bald, barfing, sad, you know, Sunday afternoon movie or whatever Hallmark movie. We, we want the happy ending. So, and one more plug for those oncologists, she was asking about repurposed medications.
Do you know who’s going to know about those?
>> Molly Jacobson: That’s the oncologist.
>> Dr. Lauren Barrow: The oncologist. It’s not me.
>> Molly Jacobson: You’re right. Right, right, right.
>> Dr. Lauren Barrow: I don’t know. I’m like, here’s your Benadryl. And if I need to manage this, I will call my oncologist friends and say, hey, you know, that’s what they do. So plug for the old oncologist. They’re great.
>> Molly Jacobson: Yeah. Well, and like you point out, the reason they know about the repurposed drugs is because they’re most in touch with the research, which is where the repurposing of drugs is happening, that somebody notices.
>> Dr. Lauren Barrow: Right.
>> Molly Jacobson: Another effect that a drug is having, and then they conduct a study to determine whether that’s what’s happening.
>> Dr. Lauren Barrow: Right.
>> Molly Jacobson: And then they continued on with the studies to develop, possibly, treatments eventually that incorporate that drug as a repurposed drug. So it’s actually the oncologists who know what’s at the forefront of the research so there’s a lot of reasons why anybody whose dog has cancer might want to consult with an oncologist even if they know they don’t want to do chemo or radiation or surgery, it’s worth it just to get that perspective from sort of the front lines of cancer treatment and research. Yeah.
>> Dr. Lauren Barrow: Sure. And you know, the other thing that they have, sorry to interrupt you.
>> Molly Jacobson: Not at all.
>> Dr. Lauren Barrow: They know the newest things that are happening. So, you know, immunotherapies and all of this cutting edge stuff, someone is doing trials on those. And when the people are doing trials, they reach out to the oncologist and say, we need patients for these trials.
>> Molly Jacobson: Right.
>> Dr. Lauren Barrow: They don’t call me. They call the oncologist and they say, Hey, we need dogs who have this kind of thing. So if you’re looking for the cutting edge, the oncologists are going to have the hookups, of where to go do that, right? That and the vet schools. And a lot of times it is the vet schools.
>> Molly Jacobson: So the last thing I wanted to just ask you about in terms of Tracie’s specific question was Palladia, because Palladia has, you know, been around for several years now and it is approved for mass cell tumors. And I don’t think people necessarily think of it as a chemotherapy, although it is, but it’s given at home.
>> Dr. Lauren Barrow: Right.
>> Molly Jacobson: It’s a pill you give to your dog. So what do you have to say about Palladia?
>> Dr. Lauren Barrow: Yeah. So Palladia is pretty handy. It’s not without side effects. It’s a pill you give, I think you start every other day and then.
>> Molly Jacobson: I think there’s like a ramp up, yeah.
>> Dr. Lauren Barrow: Base it out more as you need to. It’s not something that I’ve used a lot, but it was, I believe, developed first for mast cell tumors and they had some really great results. And sometimes they will combine it with other things too. So that also, like you said, circles back to the word chemotherapy is sort of turned into a bad word. But it’s a chemical that you use for therapy.
So it’s, it’s just one that you can use at home and it’s not without a pretty high price tag. One thing that I have heard that’s good and bad is that maybe it’s so effective that your dog will keep living for so long that you will get poor because you have to keep giving the pill. So it works great.
Your dog lives a long time and now you’re out of money. Take that as you will. But that’s one of those really cool drugs that everyone is mostly happy about and starting to use on other types of cancers now too. So again, check with the oncologist. What’s the latest on Palladia? Can I take this home? You got to wear gloves.
You got to be careful with it. You got to watch for symptoms and side effects and stuff. You got to still do the blood work periodically to make sure nothing else is happening. So it’s just another really great option among thousands. It’s endless and it’s more all the time.
>> Molly Jacobson: What are the side effects that you’ve noticed on Palladia?
>> Dr. Lauren Barrow: So I haven’t seen a lot of them, but what you’ll read about is I think usually GI side effects, vomiting, diarrhea, loss of appetite, uh, that kind of stuff. But when that is seen, usually I think they just sort of back off a little bit.
>> Molly Jacobson: Yeah. I think they lower the dose.
>> Dr. Lauren Barrow: Yeah. I think instead of every other day, they, they’ll go to less frequently as my understanding. So, yeah. It’s a handy drug. One of many. Smart people out there go talk to, you know, it’s good.
>> Molly Jacobson: Thank you so much, Dr. Barrow for joining us and taking Tracie’s call. We really appreciate your insights and advice.
>> Dr. Lauren Barrow: Yeah. Thank you.
>> Molly Jacobson: And thanks to Tracie for her question. What a great question about repurposing drugs. There is a lot of excitement every day in the medical community about some new purpose that a safe drug that’s been used for a long time that everybody knows about they find something new it can do and, oh, isn’t that exciting? And the way that science works, it’s not an answer, it’s a series of questions.
So, it can be kind of frustrating to be at the beginning of a question when there’s all of this excitement about something that’s happened and that we’ve noticed, a pattern we’ve noticed, and then they go to the lab and they try it in Petri dishes with cancer cell lines and in that very pristine and orderly environment.
Oh my gosh, it works. And then they go into more large scale studies and they look at different questions that came up in that first study and they become like really, really specific about the questions they’re asking and sometimes those studies bear more fruit. Sometimes they say, wow, this really looks like it is doing what we originally thought it was doing.
But more often than not, they realize that their hypothesis sort of falls apart. So, the treatments that a veterinarian is going to feel comfortable using are going to be ones that have been tried and true. Either there’s a lot of literature backing it up, a lot of studies that show that it’s not only effective but safe, and specific doses to use, or they’ve just been using it forever and historical usage proven out that it’s really beneficial.
So when something new comes along and your veterinarian or oncologist is skeptical, it’s not because they are anti new things. They’re actually out there looking for new things all the time. It’s just that they are rather jaded, as many scientists are, it turns out. The longer I write about and think about science, the more I realize that a lot of scientists find that their initial excitement and enthusiasm is pretty quickly put out in the harsh light of the lab and the living body doing what it does, which is not always what’s expected.
So all that to say that repurposing drugs is awesome and they’re always looking for new uses for old drugs and there’s always going to be new things that people are trying. That does not mean everything old is new again and it doesn’t mean that just because something worked in a limited study it’s going to work in your dog. So proceed with caution and know that all of this in some ways because we don’t have one cure for cancer is experimental. There’s no treatment.
You’re not going to get an oncologist to tell you that the radiation or the surgery or the chemotherapy that they offer you is 100% guaranteed because they aren’t. We wish they were. I guess that’s my thought. At the end of the day, it’s all very exciting to think about new treatments for cancer. And it’s also good to rely on what we know can have benefit and we know how to control for the side effects that inevitably occur because every cancer treatment of any type has some side effects. That’s just the way medicine works.
You can’t have a potent treatment without the risk of side effects. Follow us on the socials, engage with us, call our listener line at (808) 868-3200 and leave your question and even if your dog has already had cancer and you don’t have a question now because you’ve got the answer, if it’s one you think other people should know, call and leave the question you were wondering at the beginning of your dog cancer journey so we can make a show about it and help other people.
That’s what we’re doing here. just helping you out.
I’m Molly Jacobson. And for all of us at Dog Podcast Network, I’m wishing you and your dog a very warm, Aloha.
>> Announcer: Thank you for listening to Dog Cancer Answers. If you’d like to connect, please visit our website at DogCancer.com or call our listener line at (808) 868-3200. And here’s a friendly reminder that you probably already know, this podcast is provided for informational and educational purposes only. It’s not meant to take the place of the advice you receive from your dog’s veterinarian.
Only veterinarians who examine your dog can give you veterinary advice or diagnose your dog’s medical condition. Your reliance on the information you hear on this podcast is solely at your own risk. If your dog has a specific health problem, contact your veterinarian. Also, please keep in mind that veterinary information can change rapidly, therefore, some information may be out of date.
Dog Cancer Answers is a presentation of Maui Media in association with Dog Podcast Network.
Hosted By
SUBSCRIBE ON YOUR FAVORITE PLATFORM
Topics
Editor's Picks
CATEGORY