EPISODE 48 | RELEASED April 24, 2020
COVID-19 & Dogs: What You Need to Know About Coronavirus │ Dr. Nancy Reese Deep Dive
Are our dogs in danger from the coronavirus that causes COVID-19? Are we in danger from our dogs?? Dr. Nancy Reese, veterinarian and epidemiologist, sets us straight.
SHOW NOTES
Are our dogs in danger from the coronavirus that causes COVID-19? Are we in danger from our dogs?? Dr. Nancy Reese, veterinarian and epidemiologist, sets us straight. Whether your dog has cancer or not, this episode is a Must-Listen. Dr. Nancy covers everything from how the virus is passed to dogs, how it affects them, to how to live and love with our dogs during quarantine and what the future looks like and oh, just … so much more.
This is a fantastic Deep Dive into coronavirus and COVID-19 with Dr. Nancy Reese.
“We’ve always known, even when I was in school 20 some odd years ago, they were talking about this is going to happen someday.”
Announcer:
Welcome to Dog Cancer Answers, where we help you help your dog with cancer. Here’s your host, James Jacobson.
James Jacobson:
Welcome to Dog Cancer Answers. Our conversations are usually only of interest to people whose dogs are fighting canine cancer. But today’s show is going to be helpful to everyone who lives with and loves a dog.
That’s because it is late April 2020, and the whole world is in the middle of a pandemic due to a coronavirus and it’s causing an illness called COVID-19 — and a lot of dog lovers are wondering:
“Is COVID-19 going to hurt my dog?”
And:
“How much should I be worried about my pets?
And since this is such an unprecedented time, we thought it was a good idea to talk to our favorite epidemiologist veterinarian, Dr. Nancy Reese, and find out what we need to know and what you need to know about coronavirus and our dogs.
And don’t worry about this show being out of date, because Dr. Nancy has also written a companion article to this show, and the link to that article is in the episode’s show notes.
Dr Nancy is going to keep updating that article as often as needed to keep all of us in the know, so, check out that article after you listen to this episode.
And now, let’s go to that conversation with Dr. Nancy Reese, a veterinarian who earned her numerous degrees from the University of California at Davis.
Dr. Nancy Reese, DVM, MPVM, Ph.D. — that’s a lot of letters behind your name. Thanks for being with us today.
Nancy Reese:
Well, thank you for having me.
James Jacobson:
So let’s break down all those letters cause you’ve done 30 years of clinical veterinary experience, and you have a lot of different degrees.
Nancy Reese:
Yeah, I almost spent as much time in school as I did working as a professional.
James Jacobson:
So you got a DVM. Walk me through those different degrees cause I think it’s interesting not only because you’re so learned, but it’s also relevant to what we’re talking about today.
Nancy Reese:
So I started in undergraduate with a BS degree, a Bachelor of Science in Zoology, and then went to vet school, which is another four years to get my Doctor of Veterinary Medicine.
Then I actually went to private practice for a short bit of time. I was a little bit unhappy when I first started working in clinical practice, and I had really enjoyed school. So, while I was still working, I went back to UC Davis and got a Masters in Preventive Veterinary Medicine and enjoyed that enough to end up going back for a PhD In Epidemiology, also at UC Davis.
Of course, during that time, I was still working and decided I liked it. So, I ended up working in the same practice now for about 28 years.
James Jacobson:
Wow. And the epidemiology is going to be really relevant as we talk about COVID-19 today, because, I mean, you sort of are an expert on understanding these types of diseases.
Nancy Reese:
It certainly is a useful degree to try to piece together some of the reports that are coming out in the news stories and things. Unfortunately, it’s so rapidly changing. I mean, every study that is done a few days later, something contradicts that, because it’s so early in the understanding of this disease that, while it’s great to have the epidemiology so I can understand each study’s approach and things, it’s frustrating when you find out a few days later that the information has changed.
James Jacobson:
I totally understand. Well, you wrote an incredibly informative piece; I want to make sure we tell folks about that. It’s an article on Dog Cancer Blog, it’s called Coronavirus and Your Dog, What You Need to Know. We will have links to it in the show notes for this episode, but it is an incredibly comprehensive piece, and we’re going to kind of take it apart and talk about some of the aspects of it because I found it so fascinating. I guess the first question that people want to know is, “Can my dog get COVID-19?”
Nancy Reese:
So, at this point, there have been very few dogs that have been found to have the virus in them, so they seem to be able to possibly pick it up.
The virus itself: they can pick it up from an infected human, but so far there are no cases of sick dogs and there are no instances of dogs transmitting it to humans.
So while they, we think they can possibly get the virus if they’re exposed to — probably large quantities — from an infected person, it does not seem like they’re effective hosts and they don’t seem to get sick from it, at least not to this point,
James Jacobson:
But I do remember reading in the press reports, and there’ve been so many, that there was a dog in Hong Kong that got it from eating like, you know, a used Kleenex?
Nancy Reese:
That’s interesting. I haven’t heard how they assume that the dog got it, but that would be theoretically if there was a high dose of infective particles or lots of virus on a Kleenex and the dog did ingest it, it could possibly get infected through the mucus membranes of the mouth, but a much more common way would be to get it through respiratory secretion. So like a human really sneezing on the animal or directly infecting it would be much more likely than that sort of accidental ingestion of something.
James Jacobson:
Okay. So basically you’re saying dogs can’t really get it, but the question is, can I get COVID from my dog? Can it go the other way, from the dog to me?
Nancy Reese:
Yeah. So at this point, there’s definitely been no circumstances where we found a dog transmitting it to a human. And certainly with the number of, I mean, that’s thousands and thousands of people that are infected, I think at this point we would really have a good understanding if the dog had given it to the person.
But in all instances where they found maybe a cat or a dog exposed, it seems to be only gone from the human to the animal and not from the animal to the human.
James Jacobson: So, you mentioned a cat. Now, there’s been some press reports about cats getting it, or are there any different cautions between dogs and cats as it relates to COVID-19?
Nancy Reese:
Oh, there definitely are.
The cats, as a saying, in veterinary medicine goes, cats are definitely not small dogs, so they’re very different in the types of diseases they get, and we certainly know there’s differences in their behaviors. But the cats — there was the case of the tiger in the New York zoo that they think got it from an infected human and then potentially passed it on to a couple of the other tigers that were there.
And experimentally, they have infected cats and the cats have actually showed some symptoms. And those cats have actually been able to spread it to cats that were housed in cages next to the infected cats. So at this point, it does seem that cats could be infected with the virus, get mild symptoms, and potentially pass it to other cats.
They still haven’t found any cases where a cat has transmitted it to a human, but the cat-to-cat transmission is certainly possible. So treating a cat around an infected person would be just like treating another human around the infected person: keeping them isolated, washing hands between exposure, things like that.
James Jacobson:
Okay, well let’s get back to dogs for a minute and then we’ll talk about all the things that you can do at home to keep it more safe for you and your dog. But in terms of dogs, if you go out and you’re walking a dog and you know, dogs don’t necessarily observe the six-foot radius, social distancing, how risky is that?
Nancy Reese:
I think at this point out of an overabundance of caution, everybody is still recommending that the dogs try to maintain that social distance, particularly probably from a human more than another dog, even.
So if your dog is on a six-foot leash and your friend’s dog is on a six-foot leash, and they happen to touch noses, if they were both healthy, chances are there would be no transmission, but if one of those humans was infected, neither dog should be near anybody. So, if you’re an infected human with a dog, that dog should not be going out in public, just in that rare chance that that dog would carry it to somebody else.
James Jacobson:
Okay. So this is definitely one of those opportunities where you want to use the short leash and not the long flexible ones because, um, because those go 18, whatever, those go a long way …
Nancy Reese:
Right, those are — and they can be dangerous
James Jacobson:
Dangerous in so many ways. Normally they’re great, but not so much in this situation. Let’s talk about disinfectants and if you’re using disinfectants around the house to do all the things that we have been told we should do, do we need to worry about different disinfectants or, you know, different considerations for disinfectants when it comes to dog households?
Nancy Reese:
So a big thing is I wouldn’t apply a disinfectant directly on the dog. Mechanical bathing, grooming, things like that should be enough to reduce any possible chance of viruses that are on the dog itself.
So the virus is broken down fairly easy, even by things like soap and water. Um, so on a dog’s coat, I would only use the normal things you use to clean a dog.
Around the dog area, if it was an infected person that was shedding this virus around the environment, then certainly all the standard disinfectant types of products that are safe to use when they’re used according to label directions.
So countertops, floors, you know, any sort of surfaces that the dog might come in contact with: if there’s an infected person in the house, those should be cleaned and disinfected just to keep the dog absolutely safe.
James Jacobson:
Okay. And we know that a lot of our listeners have their dogs sleep in their bedrooms and probably often in their beds with them.
What about cuddling and sleeping with your dog, whether you’re well or if you are sick or think you might be?
Nancy Reese:
So if you are a well person and you have not been exposed to anybody that potentially has the virus and your dog has been with you and not exposed to anybody, any human that has potentially had the illness, you’re pretty safe to be handling your dog. You can have it snuggling up with you. All of those things, you’re pretty safe. As long as neither of you have come into contact with somebody that had the the virus.
If for some reason you had your dog, say you gave it to your aunt and she developed the illness and then you’re going to have the dog back.
I would out of caution, treat that as a possible infected dog and do all the things like hand washing after you touch the dog, maybe wearing a mask when you’re touching the dog.
If you’re healthy, the dog has not been exposed, you can act perfectly normal around your dog.
If you’re sick, you should isolate away from the dog.
If your dog has been exposed to somebody that’s sick, isolate the dog away from you. If that makes sense.
James Jacobson:
It totally does. So, Dr. Nancy, what about going to the vet? Now, obviously, most of the listeners to this podcast have a dog that has cancer, or they’re pretty used to going back and forth to the vet. That’s got to change in this environment.
Nancy Reese:
It definitely has. We are very fortunate that, hopefully all of the States, but I certainly know most of the States are still considering veterinary services as essential services, so the clinics can still be open to serve their clients and patients.
But we’re having to take a little bit of a different approach. And most of this is to protect both the veterinary staff from coming into contact with any humans that might be infected, and also reducing any of the potential clients coming in from anybody else that was in the clinic. So most clinics are having people pull up into the parking lot, phone when they’re there, and then the clinics will offer what’s called curbside service.
A technician or assistant will go out to the car, usually with personal protective equipment on, and take the history and get the information and then bring the pet inside, do the treatments, or contact the owner about any questions or things like that. Once everything’s done, the animal is then returned to the car, and that just minimizes any human-to-human infected people contact.
James Jacobson:
And that’s more like for regular veterinary services, right?
Nancy Reese:
True.
James Jacobson:
So I mean, should you be doing those regular checkups, those things that we’ve been told to do, go in and get the dog’s teeth cleaned and those types of things?
Nancy Reese:
Right.
James Jacobson:
What do you think?
Nancy Reese:
No. Most places are definitely limiting it to urgent care and immediate, immediate needs type of thing.
So injuries or sicknesses, anything that would require like a human urgent care facility is what most clinics are limiting to. Although it’s amazing how many phone calls we get for very minor things that we are thinking it’s because people are spending more time with their animals. So suddenly they’re noticing things that they’ve never seen in their dogs before.
James Jacobson:
Ah, well that’s interesting. Yeah. Let’s talk a little bit about that. Cause people are spending more time with their dogs and you know, certainly there’s this, a lot of memes on the internet right now are like, this is like a holiday for the dogs. Cause they’re so excited to be with us all day long. But you’re saying that they’re discovering things that they might not have seen otherwise in their dog?
Nancy Reese:
That’s absolutely seems to be the case. So we have found things.
James Jacobson:
Like what?
Nancy Reese:
Well, let’s say something as simple as a skin condition, that somebody will find a lump or bump. Sometimes that’s a good thing to find early on, but some things we can tell that they’ve actually been there probably for several months. But the person just wasn’t home enough to ever notice it.
Even things like maybe some type of limping problem. The dog might have had it for a while, and when we tease the history out of people we’ll find that they will have been noticing something, but they didn’t get to see that it affects the animal all day long. Usually they’re around them morning and night, so they don’t think the lameness might be a big deal, but suddenly when they’re watching the dog for 12 or 24 hours a day, they notice that, wow, this affects him every time he walks.
James Jacobson:
So you’re getting calls from people who are concerned about that, and then you’re able to sort of look at their history and say, no, it’s probably something that Rover’s had for a while.
Nancy Reese:
Right. And so we can advise people a lot on the phone that, well, this isn’t something that really has to come in now, we can talk about things you can do at home. But if it’s something that seems much more urgent, like the dog was running down the stairs, cried out, and now is hurt. Well, that’s obviously something that just happened.
James Jacobson:
Interesting. What about chemotherapy treatments? Obviously there’s a lot of PPE that’s required for traditional chemo treatments in a vet hospital. Are those going on as normal?
Nancy Reese:
That’s a good question. Then it really will vary with the particular treatment facility. Some of the larger places that do a lot of chemo are still going to be able to handle some of those chemo appointments.
But as you mentioned, because of the PPE involved in the ordinary usage of chemotherapy agents, those supplies — I don’t think they’re in such limitation that they can’t use them at all, but they’ve certainly become more limited because we’re really trying to save some of that stuff for the human counterparts that really need it during this pandemic.
So if it’s an ongoing chemotherapy treatment, a lot of those are still going to be able to be done, but they might change the schedule or the timing of it a little bit, depending on their ability to handle, given the PPE situation. So the best thing is to call the clinic that’s treating it and find out what they’re currently doing.
James Jacobson:
I imagine that people who are treating dog cancer right now may be doing different calculations and different calculus than they were doing prior to the COVID-19 crisis.
Nancy Reese:
What do you mean by, doing different?
James Jacobson:
Well, I’m thinking people are, maybe because they’re spending more time with their animals, they may be worried about financial situations that they weren’t worried about before, cause obviously if you’re pursuing a traditional course it’s a lot more expensive. They may be focusing more on quality of life.
Nancy Reese:
Right, and that’s absolutely true. We certainly know the economic difficulties that this pandemic is bringing is going to have lasting consequences, and we really worry about that for animal care because frankly, animal care doesn’t always get the top priority.
So that’s going to be a very big issue for anybody that’s got a newly diagnosed animal with cancer. It’s going to be a much more difficult decision to find what treatments are going to be best, and frankly, what can be afforded at that time.
James Jacobson:
And it is sort of a moving parade. Have you noticed that with your own clients, cause you’re in a pretty rural part of California.
Nancy Reese:
Yeah. So, we have a lot of people here that are out of work at this point because of the shutdown and things.
And we definitely hear about that even for some of the more minor appointments that aren’t chemotherapy related. But a lot of people are having to say, you know, I hate to say this, but we’ve got to limit what kind of tests we can do and just do the very basics to get the animal through the crisis because we just don’t know how long this might last.
James Jacobson:
Okay. This is a good time for us to take a break, but when we come back, I want to ask you about things that we can do for dogs that are in quarantine because again, we’re spending so much more time with them and try to get some tips on what we can do to make that time go by better, both for you and your dog. We’ll be right back.
So, podcast listener, here is a distressing fact: cancer is the number one killer of dogs.
One in three dogs will be diagnosed with cancer at some point in their life, and one out of two dogs over the age of 10 gets cancer.
But there is good news — and that’s: a cancer diagnosis is not an automatic death sentence.
Today’s episode of Dog Cancer Answers is brought to you by the bestselling animal health book, The Dog Cancer Survival Guide: Full Spectrum Treatments to Optimize Your Dog’s Life Quality and Longevity, authored by Dr. Demian Dressler and Dr. Sue Ettinger, who is a veterinary oncologist in New York. And in a minute, I will tell you how to get their book at a discount.
Even if your dog doesn’t have a cancer diagnosis right now, you might still want to read their book. There are so many lifestyle changes and dietary changes that you can make today to help your dog lower the risk of possibly developing cancer.
This book covers so many things, including everything that you need to know about conventional veterinary treatments — that’s surgery and chemotherapy and radiation — including how to reduce their side effects.
The book covers the most effective non-conventional options, including botanical nutraceuticals, and supplements, and nutrition, and mind-body medicine — and it also will help you analyze the options and develop a specific plan for your own dog based on your dog’s type of cancer, your dog’s age, and your financial budget, and your time constraints and your personality.
The Dog Cancer Survival Guide is available wherever fine books are sold, both online and in physical bookstores, and the book is 500 pages long. It has been described as the “Bible of dog cancer” and it offers everything that you need to know to help your dog. Here are just a few of the titles of some Amazon reviews:
someone says, “Great resource. Start here first!” that’s from Laura Delaney.
Kristen H says, “This is a must read if you don’t know where to turn”
And Patsy Norman writes, “This book is the answer to the panic that you feel when you first hear the words, it’s cancer.”
So if you would like to help support this podcast, get the Dog Cancer Survival Guidance right away, direct from the publisher — it is available in paperback and there is free shipping anywhere in the United States.
There is also an eBook edition that is obviously instantly delivered to you, and that is under $10. The website to get either the paperback book or the eBook is www.DogCancerBook.com, and, because you are a listener to this podcast, you can save 10% if you use the promo code “podcast” when you check out, you’ll save 10% — the website again, DogCancerBook.com, use the promo code podcast for 10% off that is www.DogCancerBook.com.
James Jacobson:
Welcome back. We’re talking with Dr. Nancy Reese about COVID-19 and I want to ask you, Dr. Reese: since we are spending so much more time with the dogs and we’re sort of in, you know, as I said, this is bliss for them. They’re like, “Oh, I hope you just always stay here.” Are there things that we can do to make that time seem a little bit more normal? Like it’s probably very tempting to like give them a little bit of extra treats or a lot of extra treats.
Nancy Reese:
I think that’s a very good point because when you’re sitting with your dog for maybe 12 more hours a day than you’re used to, you suddenly start seeing how insistent those big brown eyes are that are looking up at you adoringly saying, I’m starving. But definitely a really good time to use something other than food as a bonding experience.
So up to a certain point, extra walks is a great thing. Getting out in the fresh air, it’s going to reduce the dog’s stress. It’s going to reduce your stress. Get some nice fresh air, those kinds of things are great for the dog.
Now if you have an old dog that’s very arthritic or maybe a dog that’s undergoing chemotherapy, something you don’t want to do anything that is going to tax the animal and make it more difficult for them. So we don’t want to exercise them until they, they are so tired they’re just passed out on the couch.
So a little bit, you know, frequent small walks. Everybody has fun with those and definitely don’t overdo the treats. They all will beg and they all are so adorable, but it’s definitely not the time that we want to see the animals putting on five to 10 pounds.
James Jacobson:
As some people do, as well.
Nancy Reese:
Yes, yes, indeed. So lots of things you know, the animals love. This is a great time to get to see how well your animal likes home grooming, do a lot of brushing and things, although dispose of that hair quickly, especially if there’s any chance it’s been around an infected person, but a lot of grooming.
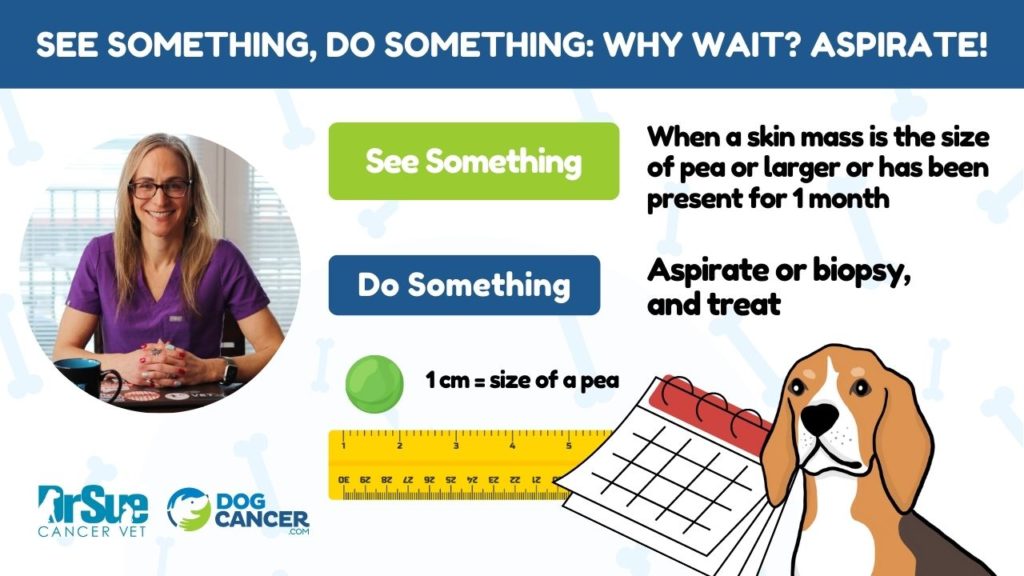
And a great time to do the lumps and bumps exam, and I think Dr. Ettinger has a really good video log on how to do one of these lumps and bumps exams.
James Jacobson:
Yeah, we did actually a podcast about the lumps and bumps where she talked about that. So check out that, we’ll put that link in the show notes to this episode along with a link to a video that Dr. Sue recorded about how to do it.
And she says, do it on a monthly basis. But of course your home, so you can do it on a monthly basis. You can find the time.
Nancy Reese:
The dogs don’t know the difference between a lump and bump check and a good rub down. So it’s a great thing for them to do and very timely indeed.
James Jacobson:
A couple of tips that I wouldn’t pass on, like my wife and I have two Maltese and we normally like go for a walk, we all four of us together.
We have found that by taking them separately, the dogs like it because there’s more quality time, just, you know, daddy and me time or mommy and me time. And also there’s less risk of running into other, you know, that whole like social distancing thing. It’s a little easier to corral one dog than it is to corral two dogs on leashes who wanted to go different directions.
Nancy Reese:
Absolutely.
James Jacobson:
And that also helps the days go by and it’s, it makes it a little bit more fun for the dogs. And then you mentioned grooming? Well, again, my wife has, we have been very blessed. We have this wonderful mobile grooming service that used to come to the house, but we don’t want that anymore.
So my wife Molly, has learned, thanks to YouTube, there are tons of videos out there. And what I thought was funny is that she gave me a haircut first to practice, and then she gave it to the dogs because they really mattered. So yeah. So you get to practice with the practice on your spouse and then, you know, do the important part of the family: the dogs.
Nancy Reese:
I’m glad to see she has her priorities straight.
James Jacobson:
She does have her priorities, but it also, again, this is probably, I can’t believe I’m sharing this — so I’m very new to this whole thing. So I had to sit in the bathtub and have her, uh, cut my hair and the dogs looked at me like “oh, okay, that’s kind of cool.”
So they figured out that’s where this happens. So it’s not the way it’s done in the salon at all.
Nancy Reese:
But see that was a good learning experience for your dogs.
James Jacobson:
That’s right, they looked a little confused and like, okay, this is where daddy gets his haircut. So it wasn’t so hard when, when they got their hair cut in the same place.
Nancy Reese:
Lead by example.
James Jacobson:
Lead by example, that’s right. Well, you know, let’s talk a little bit, cause I have seen that there are some, I don’t know if they’re myths or facts out there that some of the — this coronavirus has been around for a while, and this is where we’re going to put on your epidemiologist hat here.
Coronavirus has been around for a while and that there are actually some vaccines that have been, are used in animals that may be useful for humans, is that fact or fiction?
Nancy Reese:
Some of that is fact. The fact is that there are coronaviruses that have been with us for a long time. Currently, I think there are seven that have been identified as infecting humans, and there’s quite a few that infect different species of animals.
But the whole family of coronaviruses, each individual species in there, is quite different.
So the typical puppy coronavirus that affects their intestinal tract and gives them diarrhea is very dissimilar to the one that causes a respiratory disease in dogs, and even more dissimilar to the current one that causes the problem and people. So while they’re all called coronaviruses, they’re really quite separate viruses.
So the vaccine for the canine intestinal virus has no protection for even the canine respiratory virus, and certainly would have no impact at all on the human respiratory virus that we currently have.
James Jacobson:
Okay. We’re getting deeper into this, and I think it’s kind of interesting again, just because you are one of those rare veterinarians who has had such an academic focus on epidemiology.
What is coronavirus, and talk us through that whole process so that we have a better understanding of coronavirus and how it sort of has evolved from the animal kingdom to humans.
Nancy Reese:
If we only had all of the answers, that would be great, but we certainly have learned a lot about coronaviruses, especially since probably about the 2002, I think, was one of the outbreaks of a different coronavirus that caused a lot of worldwide concern.
So coronaviruses, there are probably hundreds and hundreds of them different versions out there, but most of them are fairly species-specific, which means that they tend to only infect and cause problems within maybe one species.
So, bats, there’re a lot of different varieties of bats. And a lot of those varieties have their own sort of unique coronaviruses. So the coronavirus that we currently have, they are thinking started in, I think it’s a horsetail bat or a horseshoe bat. So that particular coronavirus is not necessarily found in the types of bats that we have, you know, floating around our houses.
So even within a family, the viruses are fairly specific to what type of particular hosts that they like to inhabit. So at some point along the way, the virus goes from a bat to potentially another species.
And then in the case of the Middle East Respiratory Syndrome that went around, I think that was in 2002, the virus seemed to jump from bats to camels and then transformed and became infectious to humans.
So it’s quite a weird process that it can go from liking one species to changing just slightly in order to infect another species.
And then once it gets adapted to that species, it can be spread among those animals. And then in the case of those viruses that go to humans, somehow they get transmitted to humans, and then it adapts to us where we pass it onto all of our fellow humans.
So it’s long history of those coronavirus and the weird species-jumping that it does, but it’s — in consideration of all of the number of viruses are out there — it could be a lot more common than it is currently.
James Jacobson:
Interesting. Now, as an epidemiologist, you must be familiar with this whole concept of One Health.
Nancy Reese:
Yes.
James Jacobson:
What is it, and is it applicable here?
Nancy Reese:
It absolutely is, and it’s got a lot of talk in the medical fields about trying to bring, or to view, medicine as really a bigger community than just one species.
So: we were familiar with the human doctors and they treat one species, human beings, and then there’s veterinarians who treat maybe more than one species, but we all seem to have our little focus of — you know, I do dogs and cats, some of my co-veterinarians at this clinic will work on sheep and horses — so we start to expand out a little bit towards looking at multiple species, but even that isn’t necessarily a One Health approach.
The One Health approach looks at what’s happening in the environment and what are we doing that’s shifting the environment conditions that make us more susceptible to diseases.
One of the big factors that people look at is things like human encroachment into wildlife areas. By expanding out into the forest and making our presence into wildlife areas, that does several things.
One is it changes the environment itself.
It also brings us more into contact directly with wildlife, or in some cases to tick species — things like Lyme disease has been making a progressive movement from the Eastern United States further North and West, and that seems to be a direct relate to our encroachment into habitats where these ticks live.
So, One Health is really trying to get at, let’s look at the really big picture. And try to see what we’re doing that might predispose us to getting some of those infections.
If we’re going to start raiding bat caves or disrupting bat habitats, now suddenly that brings us into more contact with a species that we know really do carry a lot of viruses, which some of them seem to like to infect humans as well.
So, One Health overall is taking a much bigger picture look and seeing: not just at treating humans, let’s look at the environment and make sure we’re minimizing anything that might increase our risk to exposure to these viruses.
James Jacobson:
So as someone who studied pandemics and epidemiology, does the speed and rapidity with which this basically came across the world in any way, surprise you?
Nancy Reese:
Yes and no. Because it’s really the first one that’s had this big of an impact in what most of us that are living right now, most of our lifetimes, it does seem extremely rapid.
We’ve always known, even when I was in school 20 some odd years ago, they were talking about this is going to happen someday. We have international travel where you can get across the world in a day’s time. I mean, that really takes a huge source of infection from one country to another.
We also have, unfortunately, there’s a lot of illegal wildlife trade that goes across countries and things, and that’s a source because they’re not being screened appropriately. You can get animals carried across borders quite easily, but international travel is certainly a big one, and that obviously had some impact in this pandemic, as well.
James Jacobson:
So, what’s your — and I know you’re obviously a veterinarian — but what’s your overall sense of what’s going to happen, or when is this all going to be somewhat back to normal?
Nancy Reese:
Boy, if I could just get my crystal ball, but I think I left that at home. I think you know, they, in my opinion, now my opinion is just a humble veterinarian here, but I think people are on a good track in terms of if we can get more testing to find out truly how widespread this has been, and how many people have actually been exposed.
That’s one of the frustrating things with the numbers that come out that most of us are keeping track of, is that while we see the number infected go up, and unfortunately the number that die also seems to go up quite rapidly, we have no basis of knowing how many tests that reflects.
In my county we have a relatively low number overall, but I can’t tell you: has even 1% of the population been tested? How many sick people were just told sit it out at home unless you get worse?
So we’re on the right approach if we can test enough people to start slowly getting people cleared: people or people that have already had the infection, if we can get some of those back to work, that would be great.
But it’s really hard to see how long that’s going to be or what the next wave is going to be when we start to loosen all of those restrictions.
James Jacobson:
There is a lot of uncertainty. I guess we’re all just going to have to sit tight, stay safe, cuddle and groom and walk our dogs and our loved ones, and take good care. Dr Nancy, thank you so much for bringing your insight and your expertise and talking with us today.
Nancy Reese:
Oh, you’re very welcome. Thank you.
James Jacobson:
I want to thank Dr. Nancy Reese for that Deep Dive into COVID-19 and how it’s impacting our dogs.
I was really relieved to know that even though a few dogs seem to have caught the virus itself from an infected human, they didn’t get sick from it. It’s sad about the kitties though. That’s a tough one. The big takeaway for me is to be as careful around my animals as I am around other humans, and that we still have so much to learn about this virus.
To read, Dr Nancy’s insightful and up-to-date article on this topic, go to the show notes for this episode, which are in your podcast app or at the link DogCancerAnswers.com/coronavirus.
Questions, anyone? If you have a question for a dog cancer veterinarian, well, one of our dog cancer veterinary experts can answer that question on a future episode of Dog Cancer Answers. To make that happen, all you have to do is to call our 24 hour a day recorded listener line and record your question.
Here’s the telephone number, (808) 868-3200 that is (808) 868-3200 or you can visit us online at DogCancerAnswers.com.
And if you have an inspiring, true tale to share with us, please tell us your success story on DogCancerAnswers.com.
Also on the website, you can listen to or download our back catalog of episodes.
That is the best way to get the information that you need to help optimize your dog’s life, quality and longevity.
And in a moment, I will tell you about our next Deep Dive episode about the dog cancer diet.
But first, we would like to thank our sponsor The Dog Cancer Survival Guide book by Dr. Demian Dressler and Sue Ettinger.
The book’s available wherever fine books are sold online and in physical bookstores. And if you’d like to help support this podcast get the book today direct from the publisher Maui Media, you can get the paperback with free shipping anywhere in the USA. Or you can get the ebook edition for just $9.95. To get either the ebook or the paperback, go to this website: DogCancerBook.com. And because you are a listener to this show, if you use the promo code “podcast,” you can save 10%. The website again, DogCancerBook.com, use the promo code “podcast” for 10% off, and it’s www.DogCancerBook.com.
So on the next episode of Dog Cancer Answers, we hope you will join us because we are talking to oncologist Dr. Sue Ettinger about diet and dog cancer.
Dr. Sue — she’s also known as Dr. Sue Cancer Vet — used to be a skeptic about changing the diet of dogs with cancer, but she is a skeptic no more.
You will definitely want to hear her perspective on the dog cancer diet and what you should be feeding your dog now. It may be considerably different than what you’re doing, and so you’ll want to hear what a leading veterinary oncologist says about diet, and what you should, and shouldn’t, be feeding you pup.
And, of course, the best way to make sure that you get that podcast as soon as the episode is released is to subscribe to our podcast in Apple Podcasts or your favorite podcast app. We are also on Spotify and YouTube and pretty much everywhere that podcasts can be found.
Well, that’s it. I would like to thank Dr. Nancy for being our guest today.
Until next time, I’m James Jacobson. From all of us here at Dog Cancer Answers and Dog Podcast Network, we wish you and your dog a warm Aloha.
Announcer:
Thank you for listening to Dog Cancer Answers. If you’d like to connect, please visit our website at DogCancerAnswers.com or call our Listener Line at 808-868-3200.
And here’s a friendly reminder that you probably already know: this podcast is provided for informational and educational purposes only. It’s not meant to take the place of the advice you receive from your dog’s veterinarian. Only veterinarians who examine your dog can give you veterinary advice or diagnose your dog’s medical condition. Your reliance on the information you hear on this podcast is solely at your own risk. If your dog has a specific health problem, contact your veterinarian.
Also, please keep in mind that veterinary information can change rapidly. Therefore, some information may be out of date.
Dog Cancer Answers is a presentation of Maui Media in association with Dog Podcast Network.
Hosted By
SUBSCRIBE ON YOUR FAVORITE PLATFORM
Topics
Editor's Picks
CATEGORY